A growing body of knowledge is emerging through research at NYU Langone Health around VEXAS syndrome, a constellation of inflammatory symptoms whose origin was, until recently, a medical mystery. The condition primarily impacts men over age 50 and carries a high mortality rate.
David B. Beck, MD, PhD, an assistant professor of medicine and biochemistry and molecular pharmacology and a member of the Center for Human Genetics and Genomics, was a member of a large research collaborative that first characterized the condition—and its link to somatic mutations in the gene UBA1—by studying a cohort of patients with undiagnosed, multisystem inflammatory conditions referred to the NIH.
With his team’s latest study estimating VEXAS syndrome to be more common than previously thought, the group’s ongoing efforts are focused on identifying at-risk groups and strategies for diagnosis and treatment.
“Our research demonstrates a higher prevalence of VEXAS syndrome than more commonly recognized rheumatologic or hematologic conditions.”
David B. Beck, MD, PhD
“Our research demonstrates a higher prevalence of VEXAS syndrome than more commonly recognized rheumatologic or hematologic conditions; now it must be considered in differential diagnosis of patients who exhibit symptoms,” says Dr. Beck.
Diagnosing the Undiagnosed
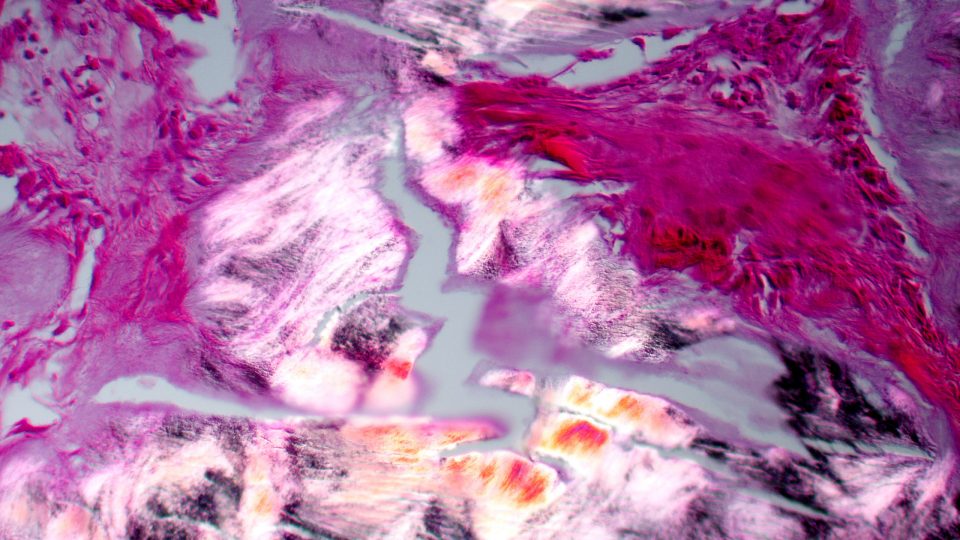
Revealed within the newly identified syndrome’s name are its associated characteristics—vacuoles in blood cells, the E1 enzyme, X-linked, autoinflammatory, and somatic.
With symptoms ranging from high fevers and joint pain to vasculitis and dermatitis, it is typically misdiagnosed as other rheumatologic or hematologic conditions until standard treatment for those conditions fails to elicit durable improvement.
“We now understand that diagnosis of VEXAS syndrome involves pinpointing a set of hallmark features—including elevated inflammatory markers and low blood counts or anemia—within a spectrum of symptoms,” Dr. Beck says.
Quantifying the Prevalence
To estimate the prevalence of pathogenic UBA1 variants in the general population, Dr. Beck and his team analyzed the electronic health records of 163,096 primarily White men and women over the age of 50 within the Geisinger Health System who agreed to have their blood screened for signs of genetic disease.
Of those screened, 9 male and 2 female individuals were found to harbor somatic variants associated with VEXAS syndrome, which correlates to 1 in 4,269 American men and 1 in 26,238 women over 50 likely to have or develop the syndrome.
Every patient genetically identified also had a clinical manifestation of the syndrome.
Building a New Care Model
Addressing the wide-ranging symptomatology observed in VEXAS syndrome demands a multidisciplinary approach involving rheumatologists, hematologists, pulmonologists, dermatologists, and other specialists.
“We’re aligning clinical resources and research to build our capacity for diagnosing and treating the condition.”
Gary H. Ho, MD
In more severe cases, the condition can cause recalcitrant thrombocytopenia and anemia in the setting of myelodysplastic syndrome, effectively a progressive bone marrow failure requiring transplant. To contain inflammation, high-dose steroids, JAK inhibitors, and other immunosuppressants can be helpful—though those treatment options are limited in their efficacy and durability.
Often, patients need to cycle through multiple medication regimens and are unable to taper from high doses of steroids without symptom recurrence.
Aligning Clinical Resources and Research
Dr. Beck and rheumatology colleague Gary H. Ho, MD, are now working to establish a referral center and a multispecialty clinic model for comprehensive care, where they can test new therapies that target the condition’s genetic basis and its associated pathways.
Their research priorities include pinpointing populations at greater risk for VEXAS syndrome, searching for additional genetic associations, and better understanding treatment responses, which Dr. Beck says becomes increasingly important as awareness of the disease increases.
“We’re aligning clinical resources and research to build our capacity for diagnosing and treating the condition,” says Dr. Ho. “The more patients referred to us, the more we hone the necessary expertise to manage their symptoms with comprehensive care.”