The expansion in therapeutic options for inflammatory bowel disease (IBD) means that more patients achieve remission and a smaller proportion require surgery than years past. The challenge now lies in identifying avenues for early intervention and tailoring therapy to optimize response, says David P. Hudesman, MD, co-director of the Inflammatory Bowel Disease Center at NYU Langone Health.
“We have multiple different treatment options, a lot more than we had just five years ago, but the challenge today is determining how to pick the right drug for the right patient,” Dr. Hudesman says.
Currently, he and NYU Langone colleagues are leading an expansive array of studies—from clinical trials focused on optimizing approved therapies to projects aimed at assembling a suite of medical and surgical risk prediction tools—to drive improvements in treatment along multiple fronts.
Optimizing Therapy
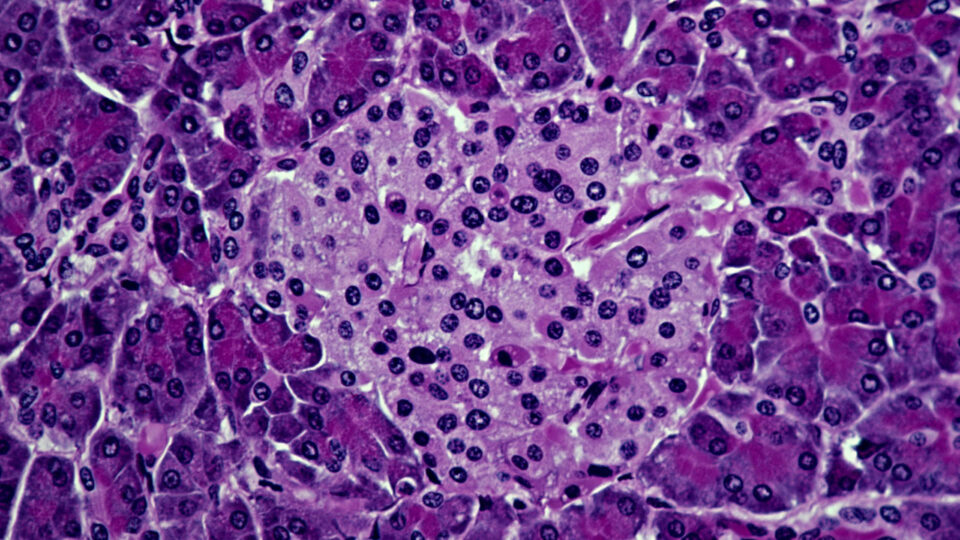
One trial that recently finished enrollment is a prospective cohort study to identify predictors of response to tofacitinib for patients with ulcerative colitis. Dr. Hudesman, who is serving as the principal investigator, says genetic data, blood immune profiles, stool microbiota, and cellular and molecular profiles of tissue biopsies are all being used to create a treatment response model.
Any predictive biomarkers identified will be validated against datasets from larger studies.
Another clinical trial led by Dr. Hudesman is evaluating the benefit of higher doses of ustekinumab early in therapy for patients with moderate to severe Crohn’s disease. “The standard dosing is not going to work for all our patients. And if we optimize drugs earlier on, we’re more likely to improve clinical remission rates,” he says.
Parallel research from Jordan E. Axelrad, MD, MPH, director of clinical and translational research at the IBD Center, and national collaborators is supporting the use of these effective agents in an expanded patient population. Their initial analysis of data from the prospective SAPPHIRE registry indicates that tofacitinib, ustekinumab and other newer immunosuppressive agents are not associated with new or recurrent cancer in patients with IBD and a recent history of cancer.
Predicting Risk
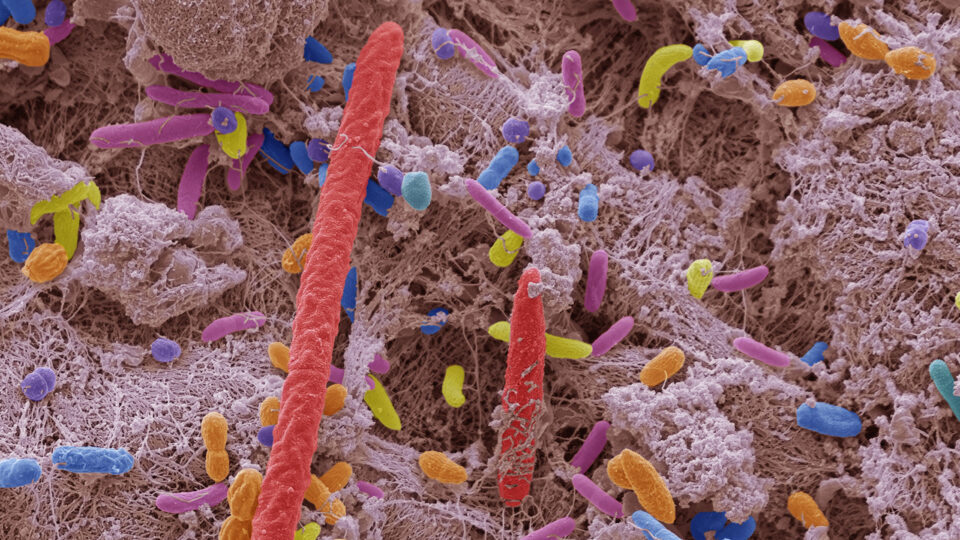
Placing focus on IBD in older adults, Adam Faye, MD, an assistant professor of medicine and population health, has found that antibiotic use is a risk factor for adult-onset disease. Older adults represent one of the fastest growing populations of patients developing IBD, with upwards of 15 percent of new cases occurring in individuals over 60.
In a study presented at Digestive Disease Week 2022, Dr. Faye and his research team analyzed data from over 2.3 million individuals aged 60 to 90, finding that a single course of antibiotics raises the risk of developing IBD by 27 percent, while five or more courses raises the risk by 236 percent. Almost all antibiotic classes were associated with the development of IBD, but those used for gastrointestinal pathogens were associated with the highest risk.
Ongoing research from Dr. Faye and colleagues, including gastroenterologist Aasma Shaukat, MD, MPH, is defining sarcopenia as a risk factor for IBD, while Dr. Axelrad recently received funding from the NIH to continue his research on enteric pathogens as environmental factors in IBD.
Getting Ahead of Complications
Investigators at NYU Langone are also researching ways to improve the success of disease-related surgery, which remains an essential treatment option for IBD, and better address extra-intestinal manifestations of the disease.
A dual-center study between NYU Langone and Cleveland Clinic led by Dr. Axelrad has determined anti-tumor necrosis factor (anti-TNF) agents to be effective at reducing postoperative recurrence of Crohn’s disease when given within four weeks of ileocecal resection. And work led by Simon J. Hong, MD, in collaboration with colleagues within rheumatology finds that two surveys validated for screening joint symptoms are effective at flagging IBD-related arthritis.
“Across our studies, we are furthering our understanding of the pathogenesis of IBD and its extra-intestinal manifestations, personalizing both medical and surgical treatment, with the hope to bring new insights into prevention of disease,” Dr. Hudesman says.