Roughly half of patients with psoriatic arthritis (PsA) achieve good outcomes with anti-inflammatory medication, says Rebecca Haberman, MD, assistant director of the Psoriatic Arthritis Center. A key unanswered question is what keeps the other half of patients from achieving the same outcome.
“One of our hypotheses is that it’s actually depression and anxiety, or mental health stressors, that are keeping patients from achieving full remission.”
She notes about 30 percent of patients with PsA have anxiety and depression, and previous research has suggested that those with depression are much less likely to achieve remission.
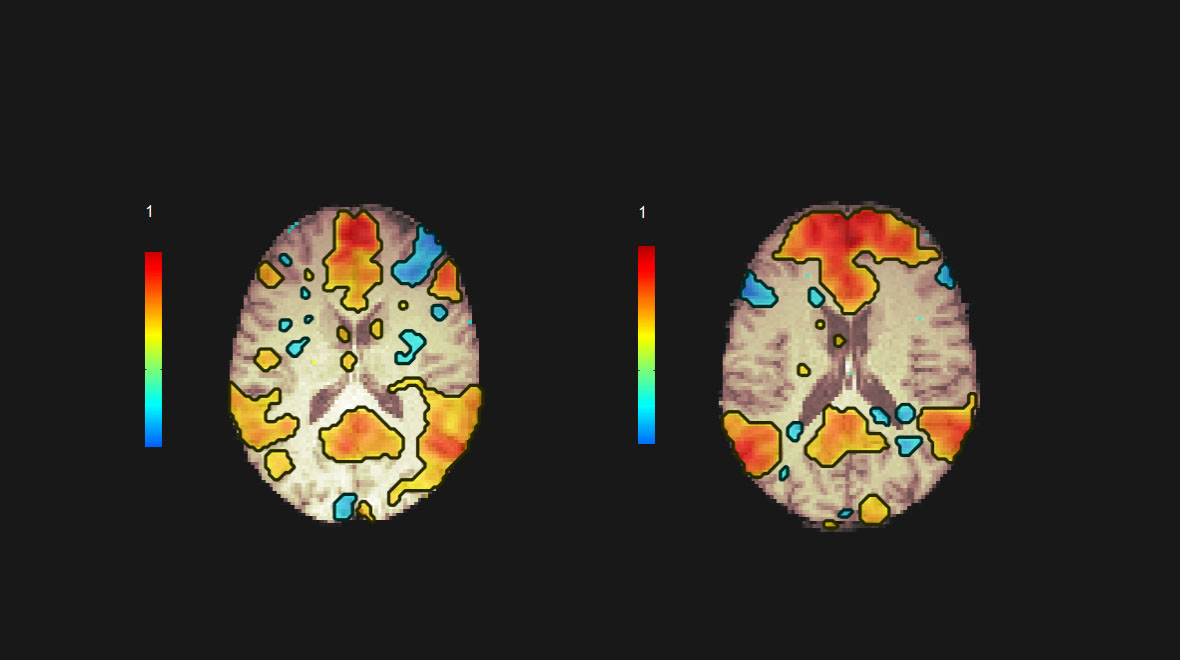
Dr. Haberman has launched a project called Mental Health and Neuroconnectivity as Predictors of Pain and Treatment Response in Psoriatic Disease. The multi-phase study is using functional MRI (fMRI) to seek out brain signals for pain, depression, and inflammation and assess whether such imaging might inform better treatment options.
“We’re often escalating their immunomodulatory therapy when the answer may be that there are other connectivity pathways that might have been altered.”
Rebecca Haberman, MD
“For patients who don’t achieve good outcomes, we’re often escalating their immunomodulatory therapy when the answer may be that there are other connectivity pathways that might have been altered and that we should be targeting,” Dr. Haberman says.
Neuroconnectivity May Influence Outcomes
The project, funded by the National Psoriasis Foundation’s More Than Skin Deep grant and the Department of Medicine Young Scholars Program, is a collaboration with Mariana Lazar, PhD, an fMRI expert in the Department of Radiology. In the first phase, they will compare imaging results of patients recruited from the Psoriatic Arthritis Center to volunteers with and without depression.
Patients will fill out depression and anxiety indices and undergo clinical exams to assess their level of inflammation. If the study establishes significant differences in neuroconnectivity, Dr. Haberman plans to compare fMRI results before and after treatment on biologics to assess whether the intervention improves the inflammatory disease and neuroconnectivity results.
Research has already shown fMRI can point out signaling pathways in the brain and distinguish among different types of depression. Preliminary studies in rheumatoid arthritis have also suggested that the disease causes alterations in brain connections that may contribute to pain sensations.
“If psoriatic arthritis, and in particular inflammation, can cause similar alterations in brain connectivity, then immunomodulatory medication alone may not be able to reverse those alterations completely,” Dr. Haberman says.
Mindfulness as a Potential Intervention
Adjuvant therapies could help normalize or reset altered neuroconnectivity pathways in PsA patients. One potential reset may be mindfulness-based cognitive therapy, which Dr. Haberman and Amanda J. Shallcross, MPH, ND, an expert on mindfulness in the Department of Population Health will explore in a subsequent phase of the project.
“We want to see if we can help reset and alter those brain connections as well as improve psoriatic disease,” Dr. Haberman says. The approach has already shown utility in improving rheumatoid arthritis.
“We know that there’s a mind-joint and a mind-skin connection… What is that connection? Can we visualize it?”
Rebecca Haberman, MD
“We know that there’s a mind-joint and a mind-skin connection,” Dr. Haberman adds. “The questions we’re trying to get at are, what is that connection? Can we visualize it, and if so, how can we use that as a tool for precision medicine?”