Patients Benefits of ESD
Gastroenterologists at NYU Langone Health are increasingly turning to an outpatient procedure to remove early cancers from the gastrointestinal tract. The procedure, known as endoscopic submucosal dissection, or ESD, is allowing more patients to avoid complex surgeries such as esophagectomy.
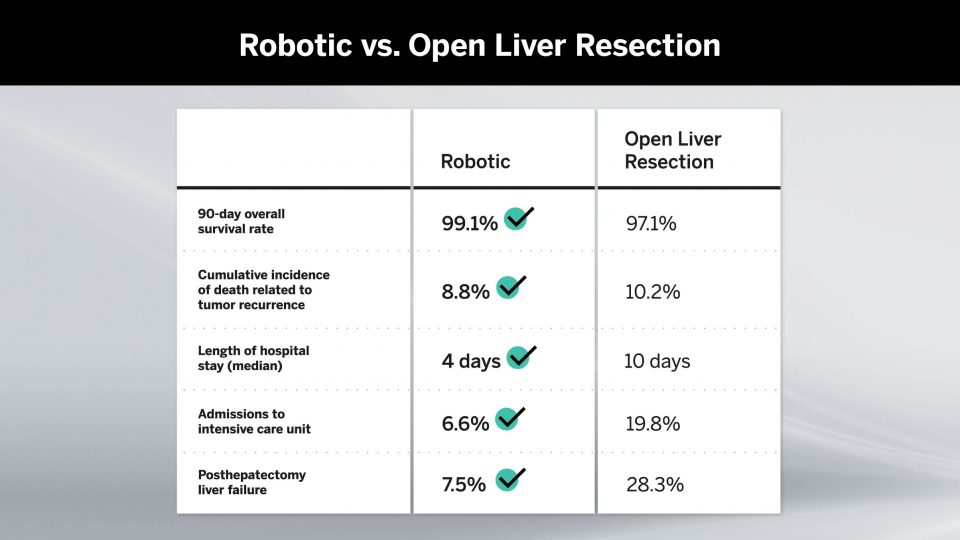
“Most patients who receive ESD are discharged the next day, after observation. This is a major difference from surgical resection which often requires an inpatient stay of up to 10 days or more,” says Gregory B. Haber, MD, chief of endoscopy and one of only a small number of physicians in the U.S. performing and teaching the highly specialized procedure.
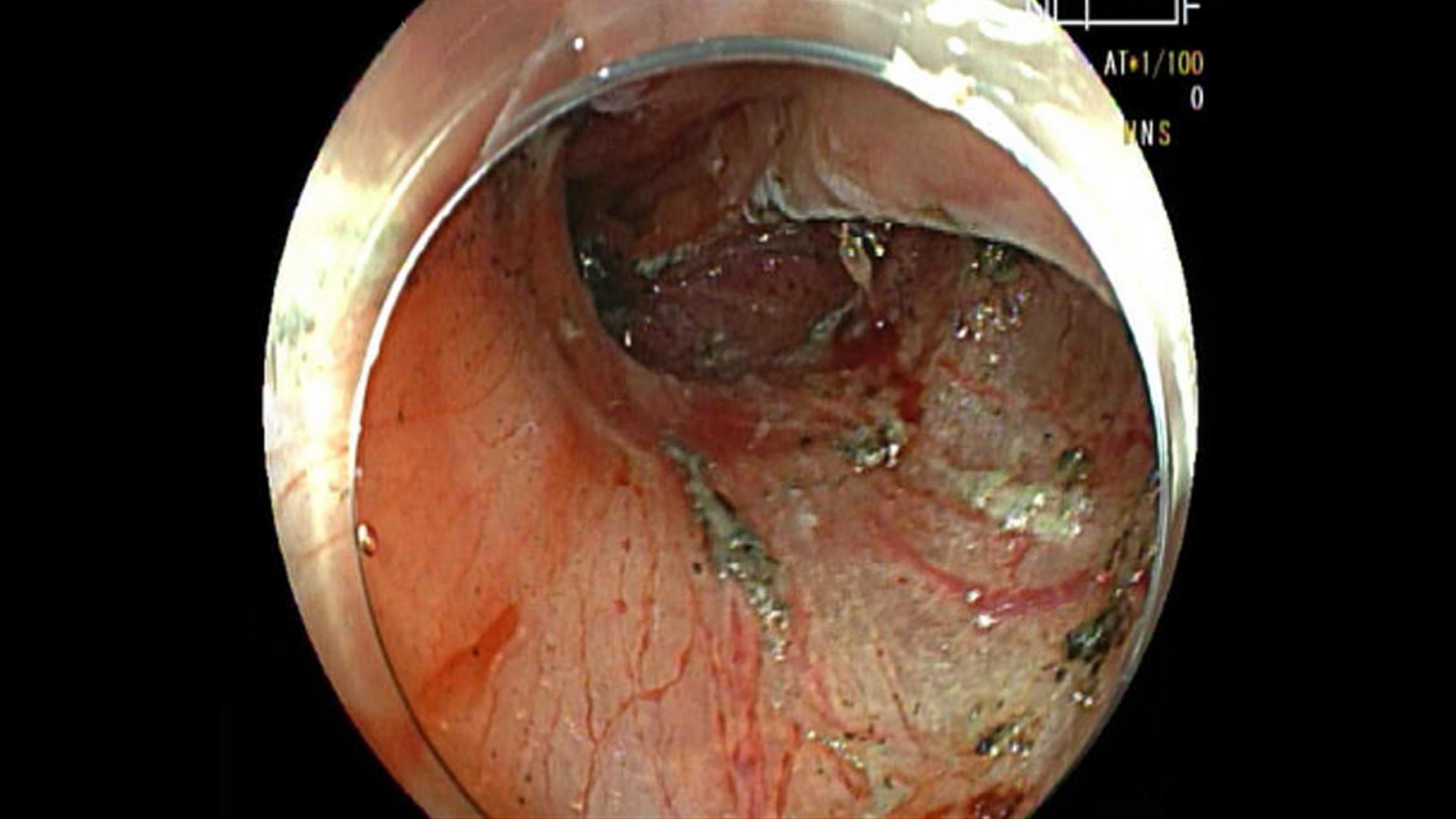
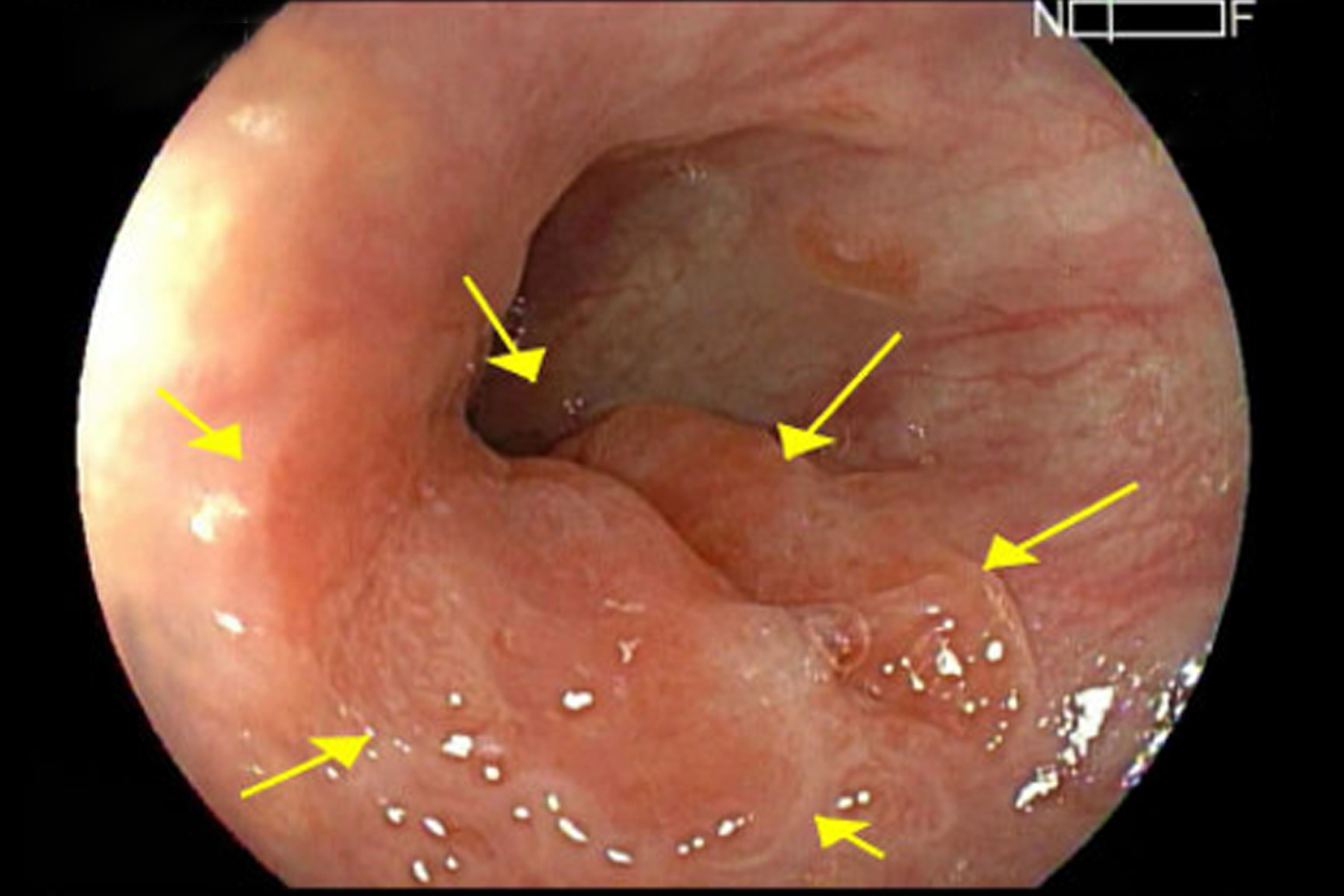
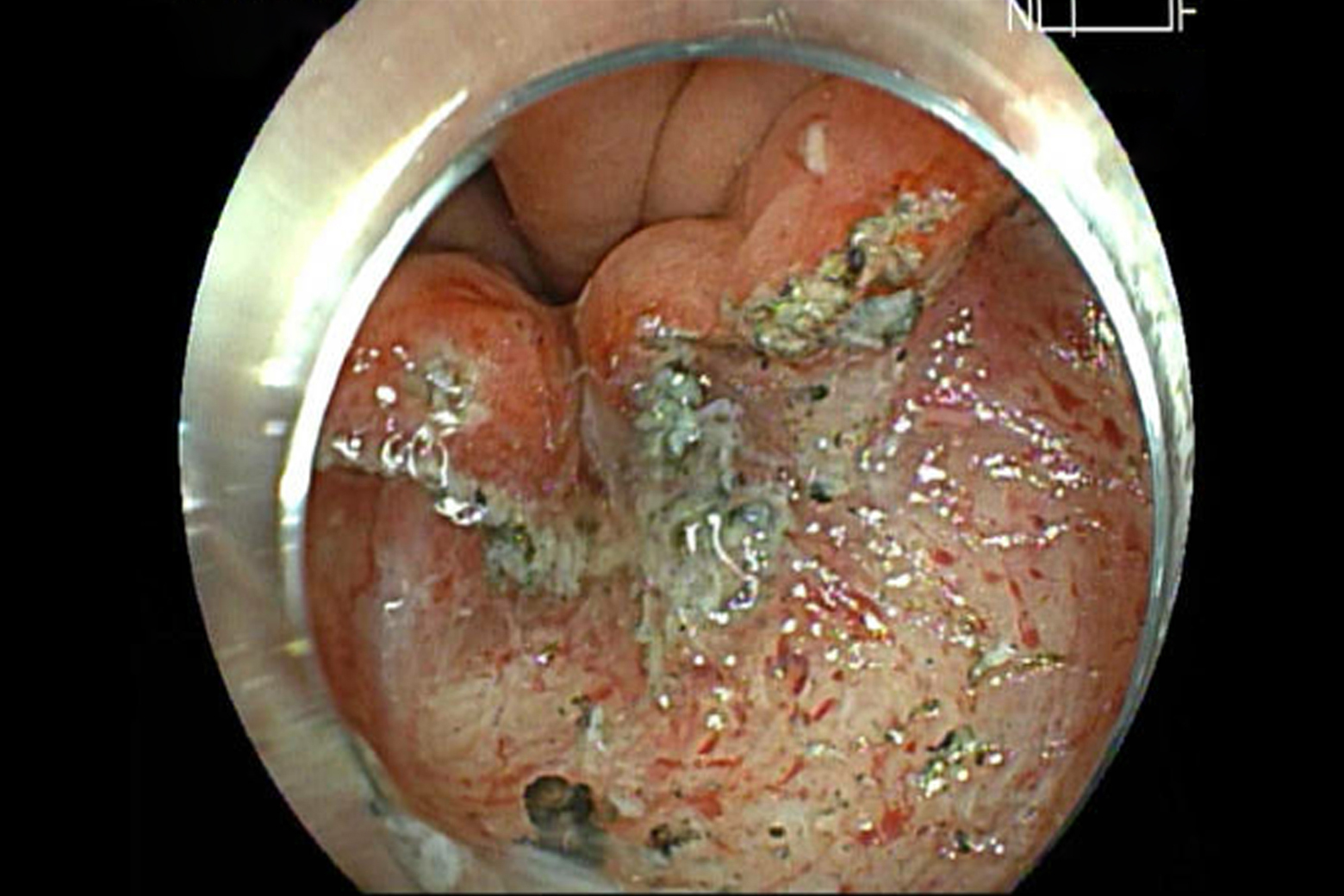
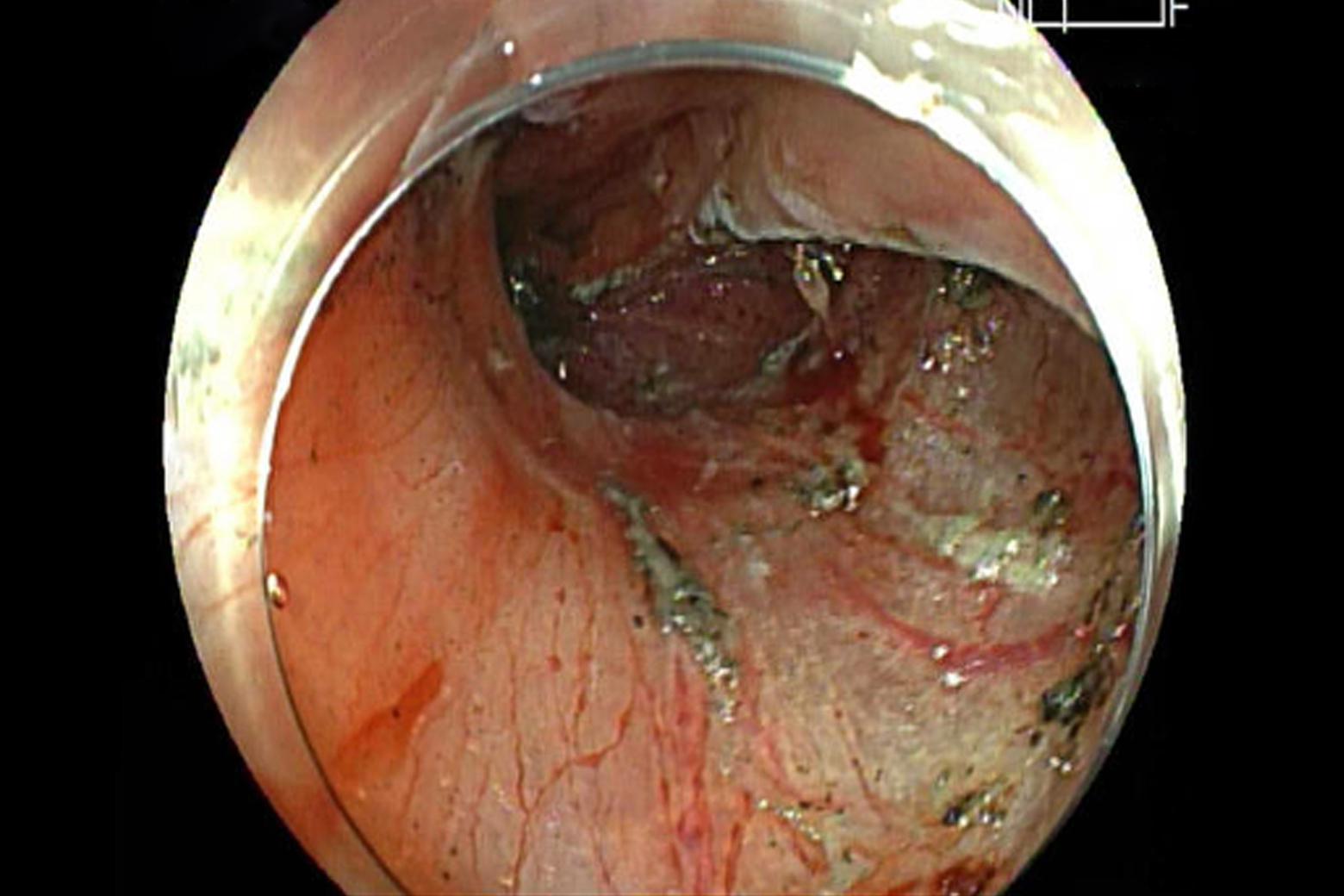
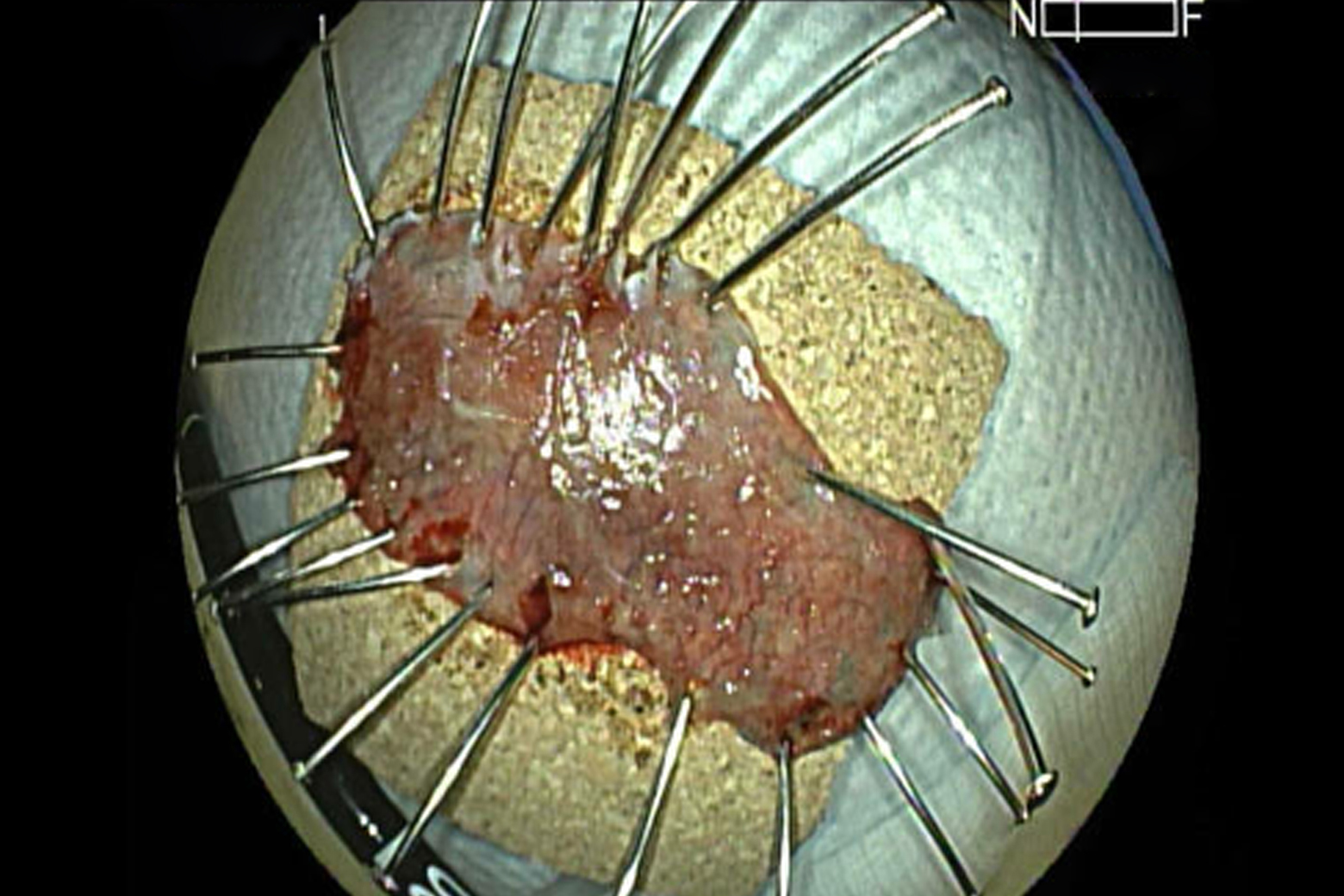
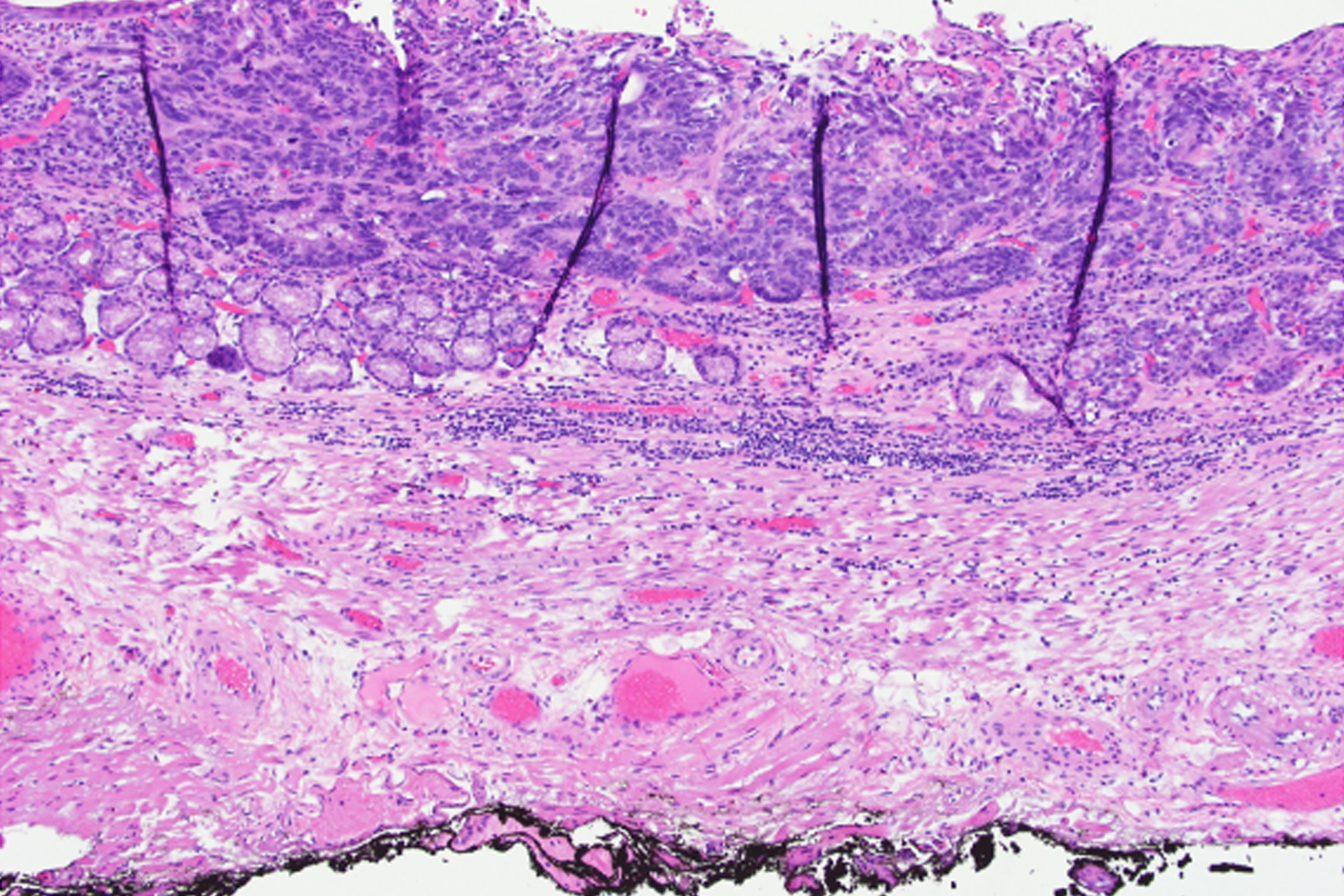
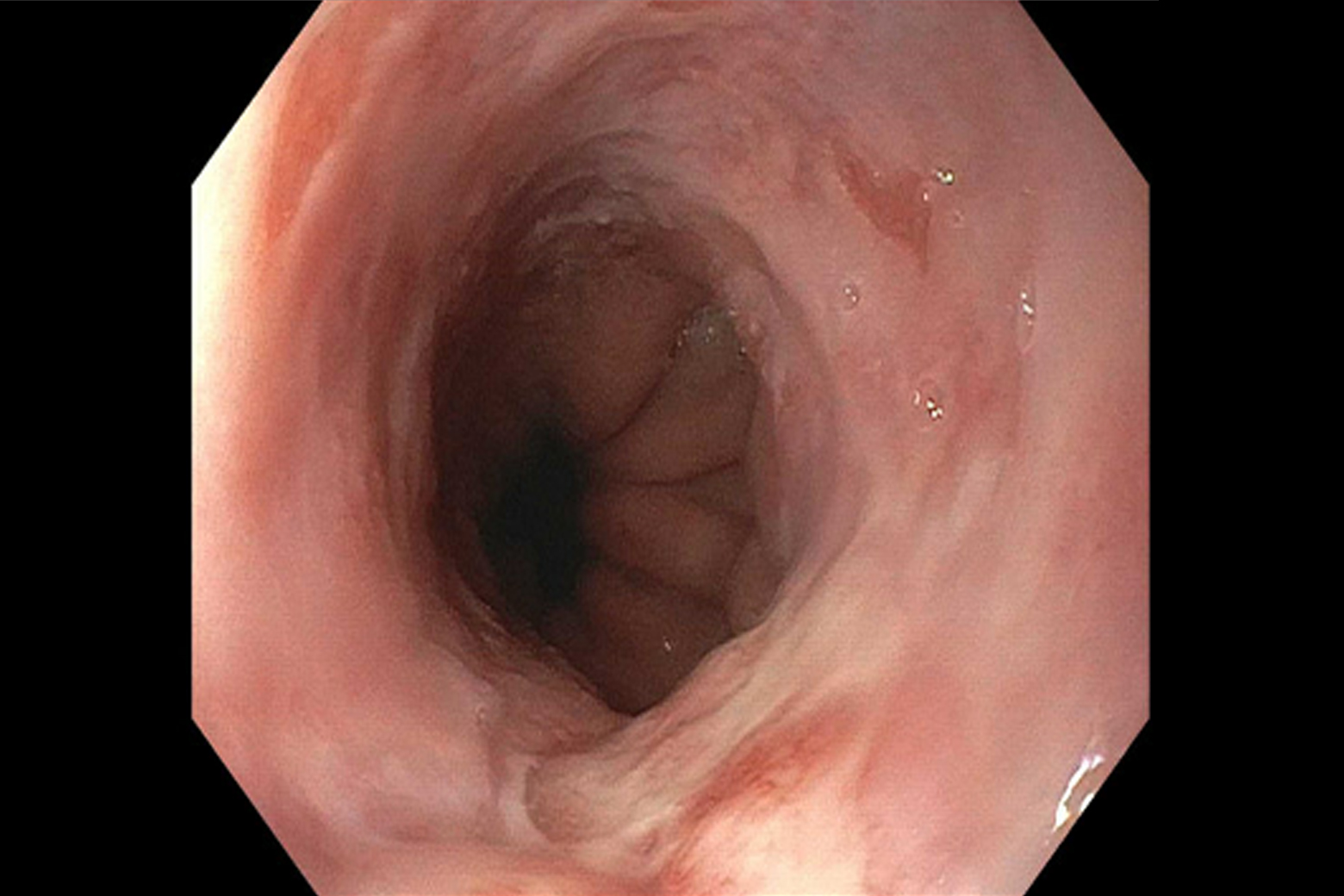
During the procedure, Haber uses a high-definition endoscope to locate and mark tumors within the esophagus, stomach, or colon of anesthetized patients. He then injects the area with a solution that includes epinephrine, hetastarch, and methylene blue to elevate the lesion and protect surrounding mucosa, before removing the whole tumor with an electrocautery knife. The approach allows a more precise resection than other techniques, Haber says.
More Nuanced Assessment
“ESD is a more effective option than endoscopic mucosal resection because it allows a deeper resection. It also allows us to remove the lesion in one piece to ensure that all cancerous cells are taken out.”
“ESD is a more effective option than endoscopic mucosal resection because it allows a deeper resection. It also allows us to remove the lesion in one piece.”
Gregory B. Haber, MD
Whole, ESD-resected tumors allow for more accurate histopathological assessment. Outcomes from ESD are also comparable to other surgical interventions, Haber says, with acute bleeding as the most common adverse event, followed by perforation, but all manageable with endoscopic treatment.
Broad Treatment Potential
Patients with Barrett’s esophagus, early-stage dysplastic cancers, or superficial tumors of the esophagus, stomach, or colon all stand to benefit from ESD. These patients would otherwise face invasive surgery to remove parts of the gastrointestinal tract.