Long-term oncologic outcomes of robotic surgery remain a topic of debate in surgical oncology, but little data has been published thus far. In one of the largest studies to date of full robotic liver resection (RLR) for hepatocellular carcinoma (HCC), researchers co-led by Karim J. Halazun, MD, section chief of hepatobiliary surgery in the Division of Hepatobiliary and Pancreatic Surgery at NYU Langone Health, found that its efficacy equaled that of open surgery—with superior results for RLR in perioperative outcomes.
“Our findings suggest that robotic liver resection confers significant advantages over open surgery in patients with HCC at expert centers.”
Karim J. Halazun, MD
Published in JAMA Surgery, the study was a retrospective analysis of prospectively maintained databases from five high-volume centers in the United States and Europe. The team evaluated both the short- and long-term outcomes of patients who underwent RLR at four of the centers between 2010 and 2020, compared with a control group of patients who underwent open liver resection (OLR) in the same time interval at an international referral center for HCC surgical management.
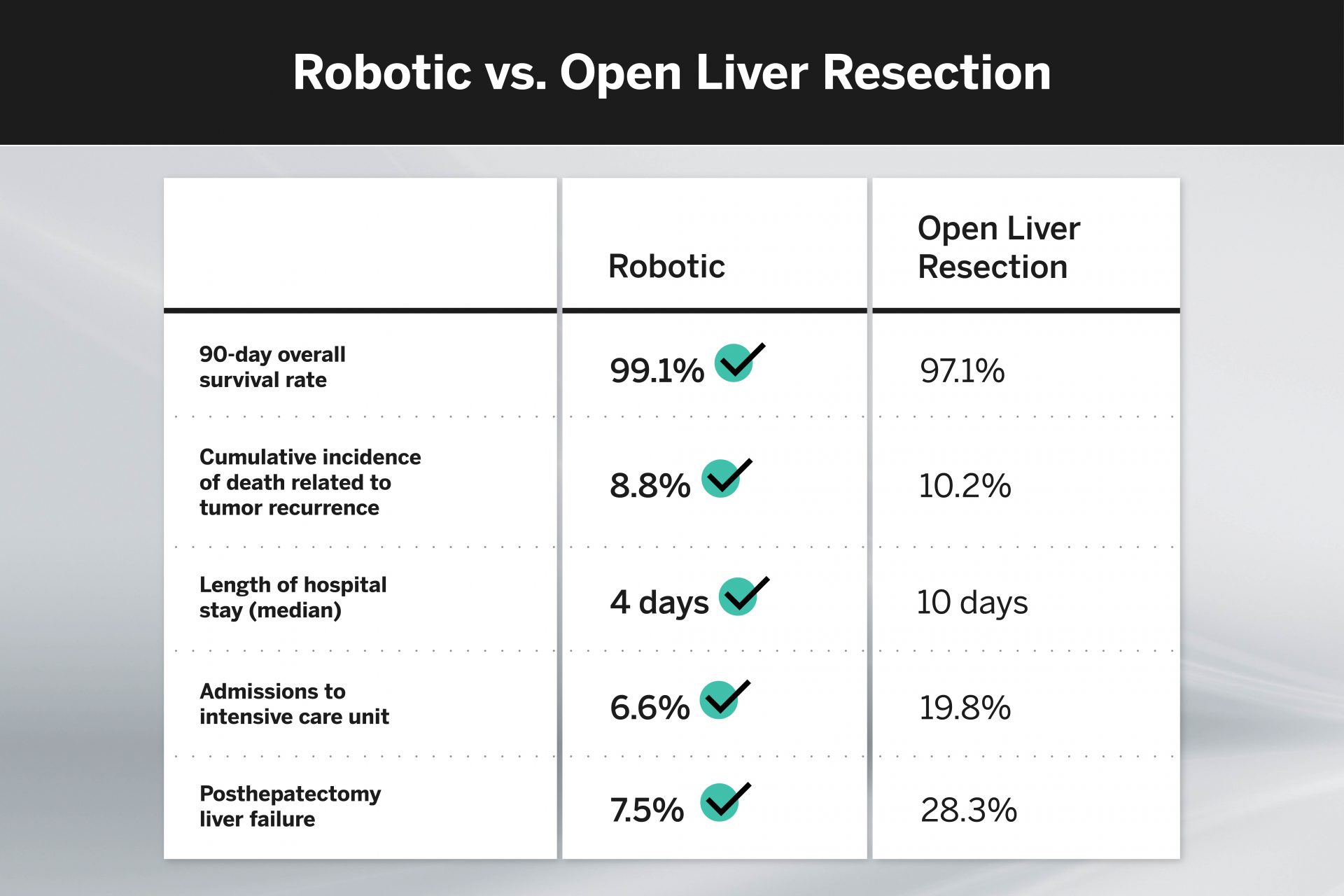
A total of 398 patients were identified in the analysis, with 158 in the RLR group and 240 in the OLR group. Overall survival rates at 90 days and the estimated overall survival rates at 24 months were similar for both cohorts, as was the cumulative incidence of death related to tumor recurrence.
In terms of perioperative tolerability, however, RLR achieved markedly better results. The median hospital length of stay (LOS) for RLR was less than half that for OLR, and admissions to the intensive care unit were two-thirds lower. The incidence of posthepatectomy liver failure was also over two-thirds lower for RLR than for OLR.
“Our findings suggest that robotic liver resection confers significant advantages over open surgery in patients with HCC at expert centers,” says Dr. Halazun. “Reduced ICU admissions and hospital LOS, as well as a lower incidence of severe complications, may ultimately lead to a reduction of overall costs and compensate for RLR’s higher technology-related expenses.
“By reducing morbidity, RLR may expand the number of patients who can receive treatment from which they are currently excluded due to the risk of liver decompensation.”