Many patients with bladder cancer are electing bladder-preserving strategies over radical cystectomy due to reservations over the procedure’s significant morbidity and impact on quality of life. A recent case at NYU Langone Health exemplifies the complexities of such a decision, with a patient with T2 muscle-invasive disease foregoing a previously planned surgery for trimodal therapy (TMT).
“This is an excellent example of how multimodal therapy can lead to treatment outcomes similar to radical cystectomy in certain patients, and with far less morbidity,” says urologic oncologist LaMont J. Barlow, MD. “Given patient interest in TMT as well as other bladder-preserving treatments, there is a great need for clinical trials designed to guide recommendations.”
Reservations Regarding Surgery
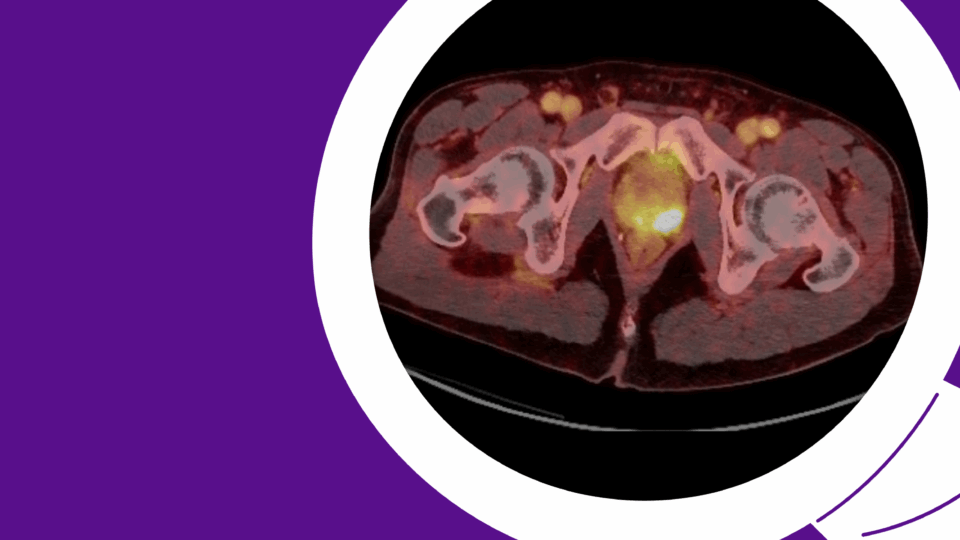
The patient, a male in his early 80s, presented with gross hematuria (>180 red blood cells), urine cytology positive for cancerous cells, and a 4-centimeter bladder mass on the left lateral wall visible by CT urography. He immediately had surgery to remove the tumor, and pathology revealed high-grade urothelial carcinoma with squamous differentiation invasive into the muscularis propria.
The patient initially agreed to have a radical cystectomy and completed four cycles of neoadjuvant chemotherapy (gemcitabine and cisplatin). With no evidence of residual or metastatic disease, he was cleared for surgery but expressed resistance to urinary diversion and an unwillingness to proceed with the treatment plan.
A multidisciplinary tumor board then deemed the patient a candidate for TMT, which the patient agreed to, viewing the chance to preserve bladder function as a welcome relief.
Success with Trimodal Therapy
Since completing TMT, which involved repeat transurethral resection followed by weekly cisplatin and 55 Gray intensity-modulated radiation, the patient has remained disease-free. The patient tolerated TMT well, developing only mild urinary hesitancy successfully managed with tamsulosin.
“This is an excellent example of how multimodal therapy can lead to treatment outcomes similar to radical cystectomy in certain patients, and with far less morbidity.”
LaMont J. Barlow, MD
Critical to success with TMT is appropriate patient selection and strict adherance to the intense treatment schedule, Dr. Barlow says.
“Candidates for TMT include patients with organ-confined muscle-invasive bladder cancer and significant medical comorbidities that would make them poor candidates for radical cystectomy, a major surgery with a high complication rate when performed by even the most skilled surgeon,” says Dr. Barlow. “Additionally, TMT is an option for certain patients with muscle-invasive disease localized to the bladder with a strong preference to avoid a urinary diversion.”
Management of disease recurrence should be discussed with patients before initiating TMT as salvage radical cystectomy may be recommended and is associated with higher overall morbidity than primary radical cystectomy, Dr. Barlow notes.
Advancing New Treatments
While there is much interest in TMT, so far no randomized controlled trial has successfully compared TMT to neoadjuvent chemotherapy plus radical cystectomy, Dr. Barlow says. Such studies, combined with ongoing trials evaluating TMT with immunotherapy, are critical next steps to guiding best practices for those with muscle-invasive disease seeking bladder-preserving treatment.