Bladder Preservation Poses a Difficult Dilemma
Having deferred radical cystectomy for years, a patient with a long history of recurrent high-risk non-muscle-invasive bladder cancer (NMIBC), who became unresponsive to bacillus Calmette-Guérin (BCG), responded well after ultimately undergoing surgery and urinary diversion.
According to Gary D. Steinberg, MD, director of the Goldstein Urology Bladder Cancer Program at Perlmutter Cancer Center, the case is representative of a common clinical conundrum—is it safe to defer or avoid radical cystectomy for BCG-unresponsive high-risk disease?
While radical cystectomy is highly curative, many patients decline to undergo the procedure due to the life-altering consequences and reduced quality of life.
“The risk of progression to muscle invasion and/or metastatic disease is greatly increased for patients with high-grade non-muscle invasive bladder cancer that does not respond to BCG,” Dr. Steinberg says. “In general, progression may occur within six to 12 months.”
The patient, a white male in his 70s, was initally diagnosed in 2011 with T1 high-grade NMIBC. In addition to BCG, his prior treatment history included mitomycin-C and interferon (IFN)-α.
“The patient reports improved quality of life with his ileal conduit urinary diversion which has eliminated his irritative voiding symptoms and incontinence episodes.”
Gary D. Steinberg, MD
After presenting to NYU Langone Health in 2019 for evaluation and management, the patient was diagnosed with BCG-unresponsive carcinoma in situ of the bladder and counselled on radical cystectomy—being the standard of care per national and international guidelines—as well as alternative therapies and clinical trials.
Aiming to preserve his bladder, the patient opted to enroll in CheckMate 9UT*. He was assigned to the three-drug arm and began treatment. When pathology revealed recurrence at six-month follow-up, the patient elected to undergo radical cystectomy and ileal conduit urinary diversion. Due to urothelial carcinoma involving the prostatic urethra, urinary diversion through orthotopic neobladder reconstruction was contraindicated.
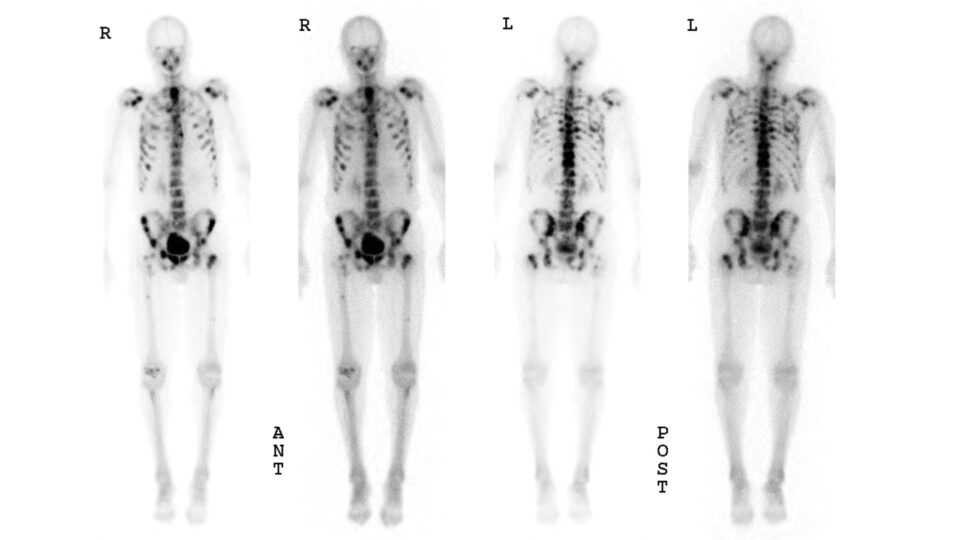
The patient regained significant function four weeks after surgery and currently shows no evidence of disease.
“The patient reports improved quality of life with his ileal conduit urinary diversion which has eliminated his irritative voiding symptoms and incontinence episodes,” Dr. Steinberg says.
*The CheckMate 9UT trial closed without reaching accrual goals due to low patient enrollment caused by the BCG shortage and the COVID-19 pandemic.