At the American Heart Association’s 2025 Scientific Sessions, renowned cardiologist Judith S. Hochman, MD, was recognized with the Research Achievement Award. The award is one of the AHA’s highest honors, celebrating transformative contributions to cardiovascular research and health.
Dr. Hochman has been recognized for her pioneering work in understanding and treating myocardial infarction and ischemic heart disease, with her landmark studies—including the ISCHEMIA trial, the Occluded Artery Trial (OAT), and the SHOCK trial—shaping clinical practice worldwide.
“I have been fortunate to collaborate with an extraordinary community of investigators, and together, we have contributed to evidence-based care.”
Judith S. Hochman, MD
Her advocacy for women’s cardiovascular health and commitment to improving patient outcomes through science reinforce her legacy as a leader in the field.
“It is a true honor to be recognized by the American Heart Association,” says Dr. Hochman, NYU Langone Health’s Harold Synder Family Professor of Cardiology. “I have been fortunate to collaborate with an extraordinary community of investigators, and together, we have contributed to evidence-based care.”
Celebrating a Remarkable Career
Dr. Hochman joined NYU Langone in 2003 as clinical chief of the Leon H. Charney Division of Cardiology and founding director of the Cardiovascular Clinical Research Center. During this period, she also served as study chair of the OAT trial and launched the Center for Multisite Studies. A founding co-director of NYU Langone’s Clinical and Translational Science Institute, she currently serves as senior associate dean for clinical sciences.
In 2011, Dr. Hochman became the study chair of the ISCHEMIA trial, designed to compare the effectiveness of an initial conservative versus invasive treatment strategy for patients with stable ischemic coronary artery disease. Funded by an $84 million award from the NIH, it was the largest grant in NYU Langone’s history up to that time.
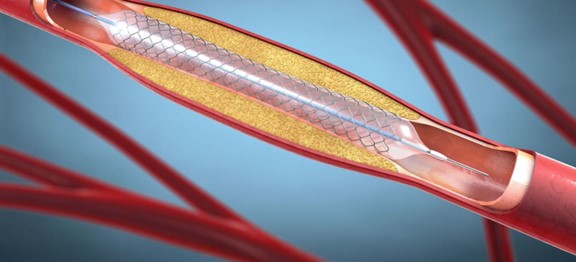
Later in 2019, Dr. Hochman presented the practice-changing results of the trial, which found that although an initial invasive strategy (stenting or surgical bypass) significantly outperformed an initial conservative approach in controlling angina, it offered no advantage in preventing cardiovascular-related death, heart attack, hospitalization for unstable angina or heart failure, or resuscitation after cardiac arrest over 3.2 median years.
To continue tracking patient outcomes, Dr. Hochman and colleagues launched an extended follow-up study, ISCHEMIA-EXTEND; interim results showed that after seven years, survival was similar regardless of whether patients began with an invasive or a conservative strategy. Although cardiovascular cause of death was reduced with an invasive strategy, that was offset by an increase in non-cardiovascular death.
A Master Clinical Trialist
Among her other major contributions, the OAT trial showed that late percutaneous coronary intervention of a persistently occluded infarct-related artery in stable patients after myocardial infarction does not improve survival or heart function and is no longer recommended in guidelines.
As study chair of the SHOCK trial, she demonstrated that early revascularization in myocardial infarction complicated by cardiogenic shock improves both short- and long-term survival. Translation of this finding into practice guidelines has improved survival for this condition. She was also the first to conduct a randomized trial of a pharmacologic agent in cardiogenic shock complicating myocardial infarction.
Within women’s cardiovascular health, Dr. Hochman was the first to report that women with acute coronary syndromes have less coronary disease than men.
“My passion has always been improving outcomes for patients through rigorous science.”
During the COVID-19 pandemic, she served as study chair for the ACTIV-4A trial (Accelerating COVID-19 Therapeutic Interventions and Vaccines 4 ACUTE) and also oversaw the CONTAIN and COMPILE studies evaluating the safety and efficacy of convalescent plasma for acute treatment of COVID-19.
Collectively, the work underscores Dr. Hochman’s commitment to employing rigorous clinical trial designs to establish clear guidance on evidenced-based care.
“My passion has always been improving outcomes for patients through rigorous science,” she says. “I am indebted to AHA for the important work it does and for my first grant, and to the NIH for its past critical support of randomized clinical trials.”
National and International Honors
In addition to this distinction, Dr. Hochman has been recognized with several other honors, including the 2008 AHA Women in Cardiology Mentoring Award, the 2014 AHA Clinical Research Prize, the 2016 American College of Cardiology Distinguished Scientist Award (Clinical Domain), the 2018 AHA James B. Herrick Award for Outstanding Achievement in Clinical Cardiology, the 2020 European Society of Cardiology Rene Laennec Award, the 2023 AHA Distinguished Scientist Award, and the 2025 AHA Critical Care, Perioperative and Resuscitation (3CPR) Dickinson W. Richards Memorial Award.