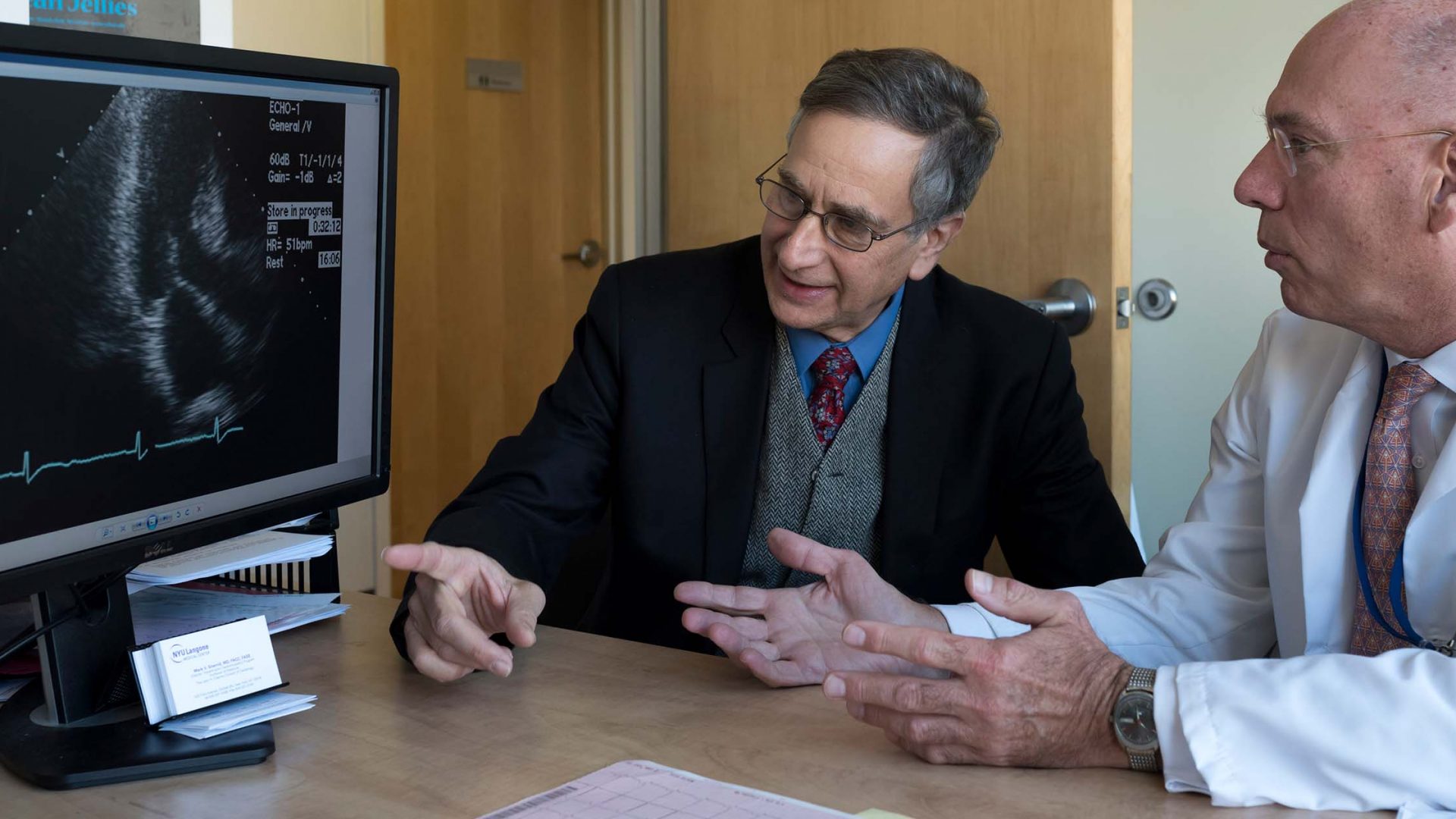
In a study published in the Journal of the American Heart Association, researchers including cardiologist Mark V. Sherrid, MD describe a previously unreported syndrome of reversible cardiogenic shock and left ventricular (LV) ballooning in obstructive hypertrophic cardiomyopathy (HCM).
A group of patients with HCM developed this syndrome, which superficially resembles an acute coronary syndrome associated with Takotsubo syndrome.
“HCM is the great masquerader of cardiology,” Dr. Sherrid observes. “In cases of LV ballooning, obstructive HCM may be overlooked because of the dramatic presentation, because the septal thickening is mild, and because obstruction may be latent. Patients are misdiagnosed with Takotsubo syndrome and given treatments that may exacerbate their symptoms.”
Affected patients had distinctive anatomical and physiologic characteristics that set them apart from Takotsubo patients. When their treatment was tailored to the underlying etiology, it was associated with favorable outcomes.
“HCM is the great masquerader of cardiology. Patients are misdiagnosed with Takotsubo syndrome and given treatments that may exacerbate their symptoms.”
Mark V. Sherrid, MD
A New Etiology for LV Ballooning
The latest study built on earlier research by Dr. Sherrid, that examined electronic health records of 44 patients diagnosed with Takotsubo syndrome. In that study, imaging showed that 30 percent of this cohort had undiagnosed obstructive HCM, indicated by abnormalities of the ventricular septum and mitral valve with systolic anterior motion of the mitral valve (SAM) and high LV outflow gradients. Observations of this group suggested that acute LV outflow tract obstruction may cause ballooning.
In the new study, Dr. Sherrid and his team analyzed 14 patients who were admitted with obstructive HCM and abrupt presentation of cardiogenic shock with LV ballooning. These patients received treatment addressing their HCM and outflow tract obstruction rather than that typically administered in Takotsubo cases.
Shock management included intravenous phenylephrine, norepinephrine, beta blocker, and vasopressin. A subset of patients in refractory shock received urgent relief of obstruction by myectomy (n=5) or alcohol ablation (n=1). Despite the typically poor prognosis for cardiogenic shock, all patients survived, with full recovery of systolic function
A Dangerous Masquerade
In cardiogenic shock associated with LV ballooning in HCM, medical therapies commonly administered in Takotsubo syndrome—such as dobutamine, nitrates, or ACE inhibitors—are contraindicated.
The efficacy of surgical intervention in cases of refractory cardiogenic shock also distinguishes the new syndrome from Takotsubo, in which ballooning occurs in the absence of underlying anatomical defects.
“This clinical scenario is one of the few in HCM requiring emergent surgical intervention,” says Daniel G. Swistel, MD, a coauthor of the most recent study. “Decisions must be made in hours, and misdiagnosis of the true pathophysiology can result in fatal missteps.”
“This clinical scenario is one of the few in HCM requiring emergent surgical intervention.”
Daniel G. Swistel, MD
The Importance of a Trained Eye
Dr. Swistel notes that the clinical definition of HCM has recently expanded to include patients who have mild or normal LV thickness, yet have outflow tract obstruction at rest or after exercise responsible for typical heart failure symptoms. These patients have mitral leaflet elongation, papillary muscle abnormalities, and SAM, but their HCM may go undiagnosed due to the lack of obvious septal thickening.
The finding that the condition can be associated with LV ballooning and cardiogenic shock “underscores the need for clinicians to familiarize themselves with the many anatomic variants found in HCM,” he observes.
“This is a huge discovery on Dr. Sherrid’s part,” Dr. Swistel adds. “It’s a real leap forward in diagnosis.”