Referral Notes:
- NYU Langone’s new Center for Molecular Oncology intends to provide molecular analysis and serial liquid biopsies for all patients diagnosed with cancer.
- To maximize insights, Marcin Imielinski, MD, PhD, and colleagues are leveraging whole-genome sequencing to enhance mutation detection beyond standard targeted gene panels.
- As an example of how whole-genome sequencing can expand knowledge, Dr. Imielinski’s lab used the technique to identify a new class of HR-deficiency-enriched rearrangements.
-
The goal is to translate whole-genome data into actionable, EMR-integrated reports that clinicians can easily interpret for personalized treatment decisions.
A growing body of evidence supports the potential of routine molecular profiling of tumors as a transformative practice in oncology. In addition, liquid biopsies—tests that detect DNA shed by tumors into the bloodstream—are emerging as a crucial tool for monitoring malignancies over time. Yet these molecular approaches are currently used almost exclusively for advanced disease, or for the small minority of cancers in which precision therapies are indicated as a first-line treatment.
NYU Langone Health’s new Center for Molecular Oncology, launched in October 2024, is pioneering a care model in which both practices play a far broader role. In the near future, all patients diagnosed with cancer throughout the health system will receive a molecular analysis of their cancer, followed by serial liquid biopsies as needed. And to help maximize the utility of such assays, researchers attached to the center are turning to a cutting-edge methodology: whole-genome sequencing.
“With standard-of-care diagnostic tests, we’re looking at a thousandth of the genome. By looking at the whole genome, we can detect and analyze many more mutations that may be therapeutically as well as biologically important.”
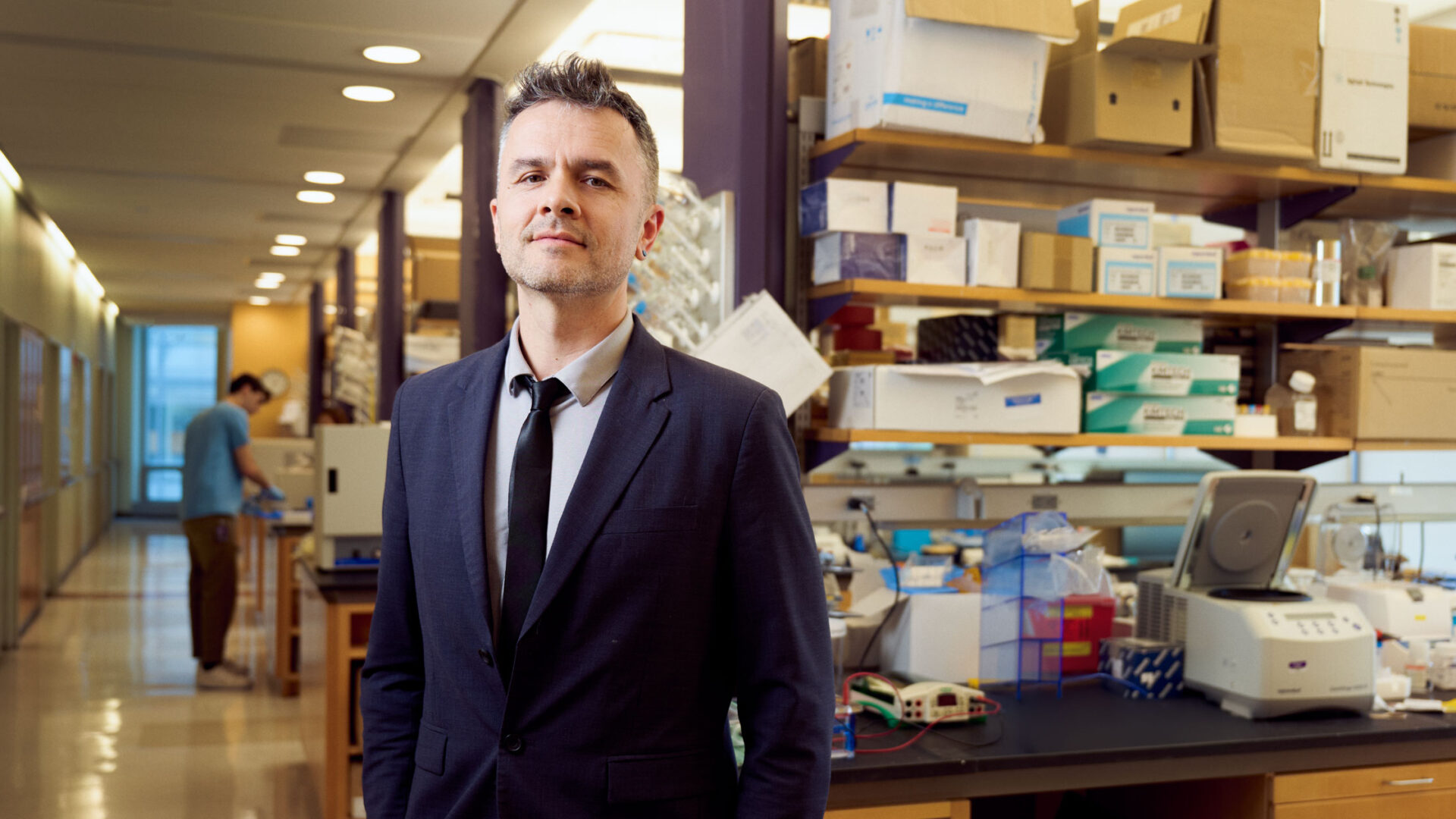
Marcin Imielinski, MD, PhD
Spearheading that effort is Marcin Imielinski, MD, PhD, director of cancer genomics at Perlmutter Cancer Center. “With standard-of-care diagnostic tests, such as targeted gene panels, we’re looking at a thousandth of the genome,” Dr. Imielinski says. “By looking at the whole genome, we can detect and analyze many more mutations that may be therapeutically as well as biologically important.”
Hunting for Key Mutations That Targeted Panels May Miss
Over the past two decades, targeted gene panels have become the gold standard for genomic assessment of cancer. The most advanced approach uses next-generation sequencing technology to test hundreds of genes simultaneously for known biomarkers of cancer. Although known as “comprehensive” genomic profiling, this method can detect only preselected gene variants.
Whole-genome sequencing, by contrast, analyzes an entire genome—whether that of the patient, the patient’s tumor, or both—for variants that may prove relevant to an individual’s cancer or its treatment, even if they are not currently recognized as clinically significant. Advanced computing techniques, such as machine learning, are employed to identify both known biomarkers and variants worth investigating further.
At present, this methodology is confined mostly to research labs. Regulators have approved a handful of clinical applications—acute myeloid leukemia in the United States, and select cancers, including pediatric cancers, in Europe and Australia—but the routine use of whole-genome tests has yet to enter mainstream oncology practice.
Dr. Imielinski, who joined NYU Langone in 2022, is a molecular pathologist with an extensive background in computational biology and genomics, and a nationally recognized leader in efforts to bring whole-genome-based diagnostic methods into cancer care. His research focuses on developing new algorithms and technologies for analyzing a tumor genome’s structure and biochemistry.
“My lab is working to identify genetic biomarkers that point to new therapies, or that can determine whether existing targeted drugs or immunotherapies could work for patients who are not now considered candidates,” he explains. “Those biomarkers could also help us determine which patients would be best suited for which clinical trials, potentially benefiting both the individual and the search for better cancer treatments.”
Beyond DNA “Typos”
To find such markers, Dr. Imielinski and his team look beyond the small “typos” in DNA, which is what many standard clinical assays and algorithms use to detect and characterize tumor cells. Instead, they investigate more-complex changes, such as rearrangements, copy number alterations, and the folding patterns of abnormal genomes within the nucleus of tumor cells. “It’s amazing that cancer cells can even survive with such deranged genomes,” he says. “Learning how they do so will help us find new ways to detect and destroy them.”
“It’s amazing that cancer cells can even survive with such deranged genomes. Learning how they do so will help us find new ways to detect and destroy them.”
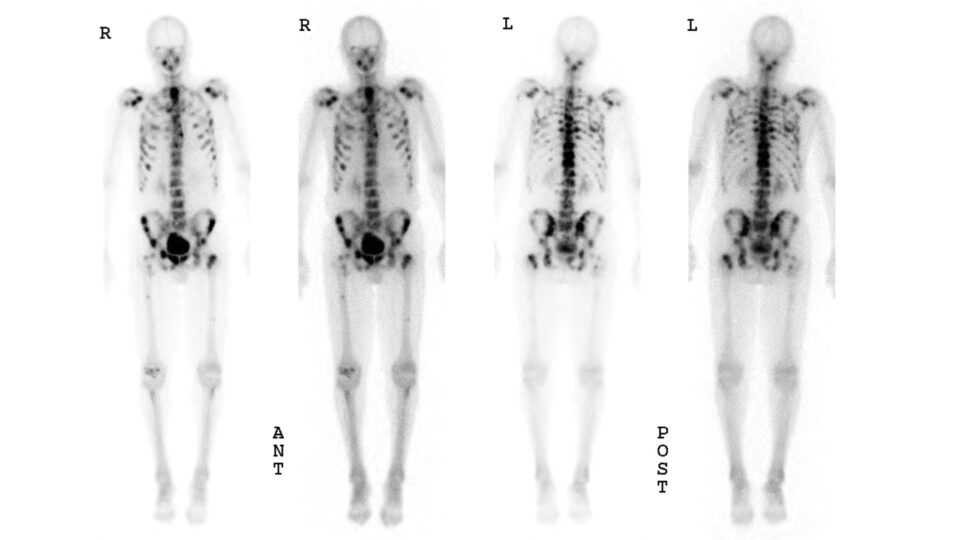
In a recent Nature study, for example, Dr. Imielinski’s lab used whole-genome sequencing to investigate the mechanisms behind homologous recombination (HR) deficiency, which is associated with faulty DNA repair. As a result, HR deficiency—and therefore susceptibility to certain DNA-damaging drugs—can be diagnosed by identifying characteristic patterns of mutations around the genome.
Analyzing the genomes of thousands of BRCA1- and BRCA2-deficient cancers, the researchers identified a previously unknown class of HR-deficiency-enriched rearrangements that can only be detected by whole-genome sequencing. Identifying tumors with these rearrangement patterns indicates specific backup repair mechanisms that may point to new therapeutic strategies for HR-deficient cancers.
Translating Laboratory Findings into Clinical Breakthroughs
Eventually, whole-genome-based methods could lead to more comprehensive molecular testing of tumors and to new drug targets, enabling personalized therapies to become standard of care for a wide variety of cancers. A whole-genome approach could also bring liquid biopsies that are more sensitive and specific, allowing earlier detection of metastases or relapses—and surer judgments of when treatment can be safely ended—than is possible with current tests.
One reason for optimism, Dr. Imielinski observes, is the increasing affordability of whole-genome sequencing. “Until recently, the cost of sequencing a cancer genome was $5,000 to $10,000,” he says. “Thanks largely to expiring patents, costs have decreased fivefold, and they could fall below $100 in the next five years.”
To make whole-genome cancer testing a practical reality, however, such assays and their reports will have to be tailored to the day-to-day needs of clinicians and healthcare systems. For this task, Dr. Imielinski and his colleagues can draw on deep institutional experience.
In 2021, the Food and Drug Administration approved the NYU Langone Genome PACT (Profiling of Actionable Cancer Targets) test, a novel sequencing tool that detects changes in 607 genes simultaneously. Designed by Matija Snuderl, MD, director of molecular pathology in the Department of Pathology, the test converts complex data into a report that includes a suggested diagnosis and recommended treatments. It matches patients with approved therapies for a variety of solid tumors, with promising experimental treatments, and with ongoing clinical trials. And it seamlessly integrates with electronic medical records.
Dr. Imielinski is working with Dr. Snuderl and other members of the Genome PACT team to follow a similar route to bring whole-genome-based tumor tests and liquid biopsies into routine clinical practice at NYU Langone.
“In the United States, no other academic health system has taken the leap to this paradigm,” he notes. “We want to show that it works and to provide evidence that other people can follow.”