Since many patients with chronic pulmonary conditions experience poor disease control, researchers are turning to the extra-esophageal manifestations of gastroesophageal reflux disease (GERD) to look for clues that might explain this phenomenon.
Investigators at NYU Langone Health’s Center for Esophageal Health were prompted by recent findings to further examine the association between GERD and chronic lung disease severity. The new research will be presented at a national conference in late 2023.
“We have evidence from pH testing that many patients with complex pulmonary disease experience a significant amount of reflux, but it’s often silent, due to the absence of symptoms,” explains Tanuja Damani, MD, surgical director of the Center for Esophageal Health.
“Overall, there should be serious consideration for low-risk minimally invasive surgery in select patients with complex pulmonary disease. These procedures are very safe and may lead to a significant improvement in disease control.”
Tanuja Damani, MD
“For these patients, the influence of GERD and esophageal motility disorders is becoming increasingly recognized, and recent advances in diagnostic testing can help to identify those who might benefit from treatment, either medically or surgically,” says Abraham R. Khan, MD, medical director of the center.
Inflammation Exacerbates Lung Disease
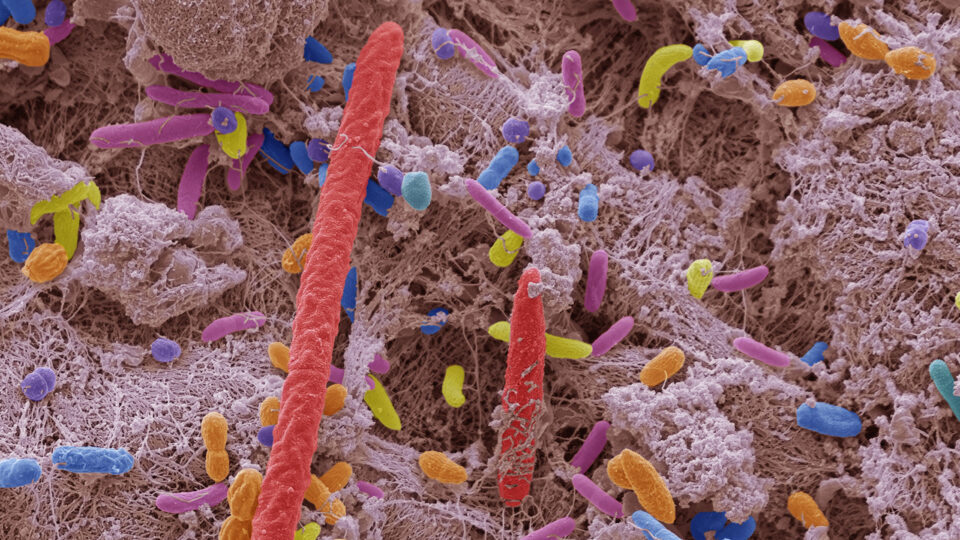
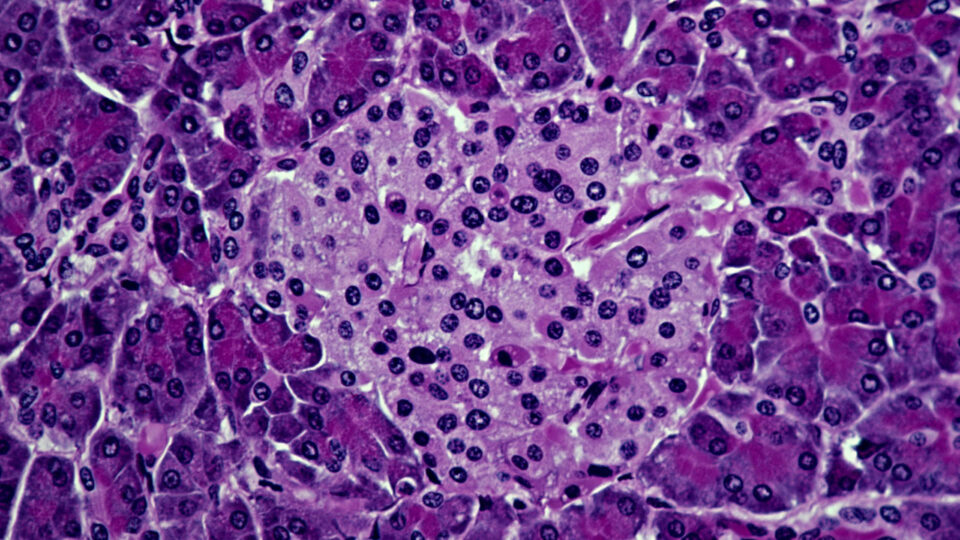
GERD is known to cause, trigger, or exacerbate many chronic pulmonary diseases including asthma, interstitial pulmonary fibrosis, and bronchiectasis, and while the physiological link between GERD and lung disease severity has been well established, it remains an underrecognized and undertreated comorbidity.
While some patients will report symptoms, including heartburn, regurgitation, and dysphagia, others may have clinically silent disease, which is frequently seen among lung transplant recipients.
“Microaspiration from reflux can lead to basilar changes in the lung tissue, driving inflammatory processes and the development of fibrosis,” Dr. Damani says.
The Importance of Testing
When evaluating patients with pulmonary disease, a personalized approach should be taken to identify the influence of esophageal disease, which may involve several different types of tests, Dr. Khan explains. For example, an esophageal manometry test or assessment by functional luminal imaging probe (FLIP) on endoscopy could be used to help identify esophageal motility problems.
“Recent advances in diagnostic testing can help to identify those who might benefit from treatment, either medically or surgically.”
Abraham R. Khan, MD
Another common test is an ambulatory pH study, which can either be done with a wireless pH-sensing capsule that examines acid reflux for 48 to 96 hours, or with a 24-hour catheter-based pH impedance test that looks at both acid and nonacid reflux for 24 hours.
“These tests are usually performed when initial endoscopic investigation is unrevealing, especially when symptoms persist despite empiric therapy,” Dr. Khan says.
Developing a Treatment Strategy
Notwithstanding lifestyle modifications and acid suppressive therapy, many patients with chronic pathologic GERD and complex pulmonary disease may benefit from minimally invasive anti-reflux surgery, Dr. Damani explains. The Toupet (270 degree) fundoplication has been shown to be as efficacious as the Nissen (360 degree) technique, but with fewer rates of postoperative dysphagia and gas bloat syndrome.
Additionally, among lung transplant populations, anti-reflux surgery has been shown to reduce the risk of chronic allograft dysfunction, but surgery has not been extensively studied in bronchiectasis other than a few reports that signal toward lung function preservation.
“In patients with bronchiectasis, GERD is an important risk factor for recurrent microaspiration and progression of pulmonary disease. The opportunity to treat the underlying GERD should not be overlooked.”
Doreen J. Addrizzo-Harris, MD
“In patients with bronchiectasis, GERD is an important risk factor for recurrent microaspiration and progression of pulmonary disease,” says pulmonary and critical care physician Doreen J. Addrizzo-Harris, MD. “For many of these patients with recurrent exacerbations and progressive respiratory compromise, the opportunity to treat the underlying GERD should not be overlooked.”
“Overall, there should be serious consideration for low-risk minimally invasive surgery in select patients with complex pulmonary disease,” Dr. Damani says. “These procedures are very safe and may lead to a significant improvement in disease control.”