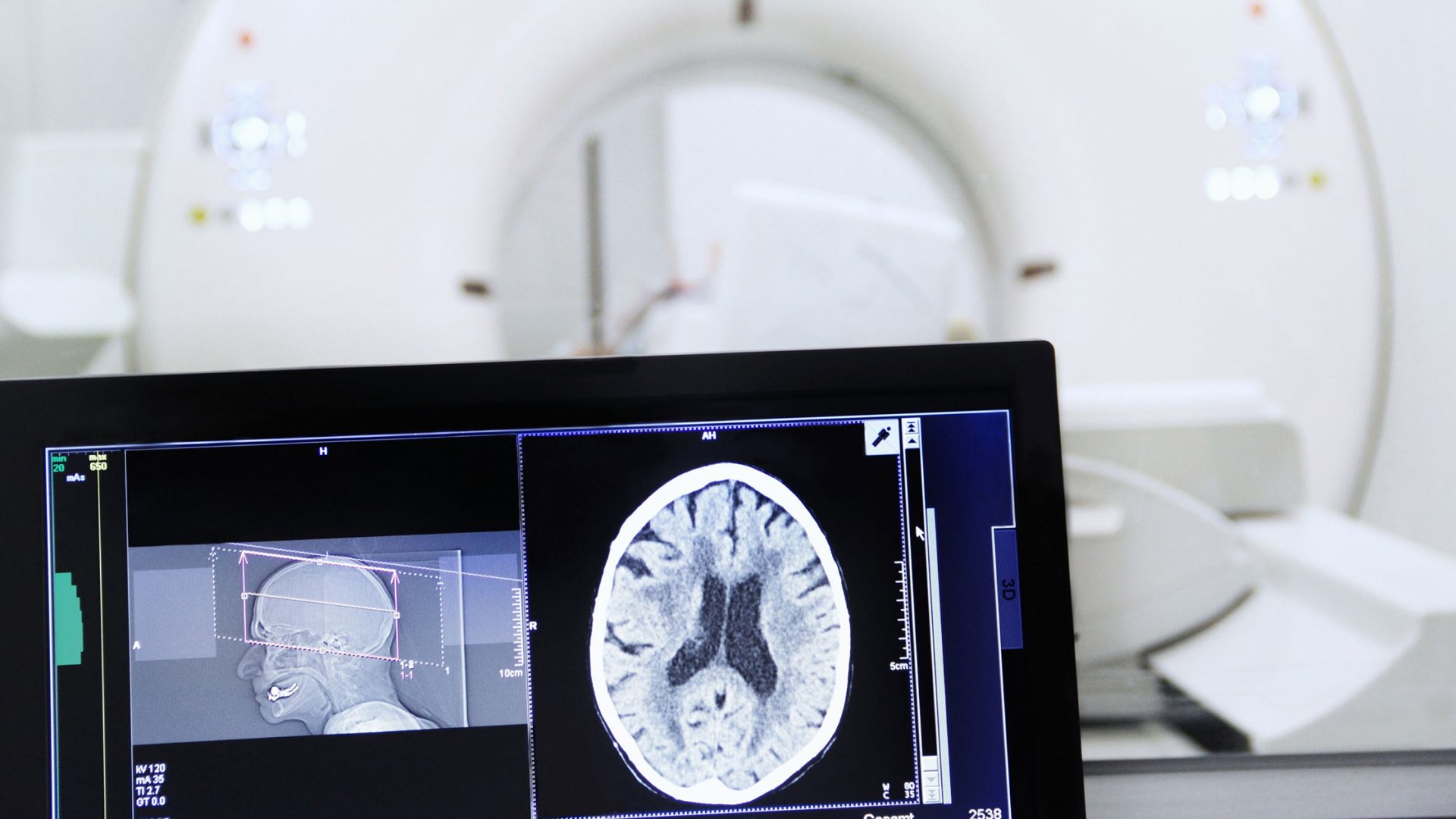
Advances in Stereotactic Radiosurgery (SRS) over the past several decades have allowed cancer patients with multiple brain metastases to be treated using single or multiple fractions of radiation therapy. NYU Langone Health utilizes specialized Gamma Knife® SRS, and is a world leader in clinical and research application of this technology.
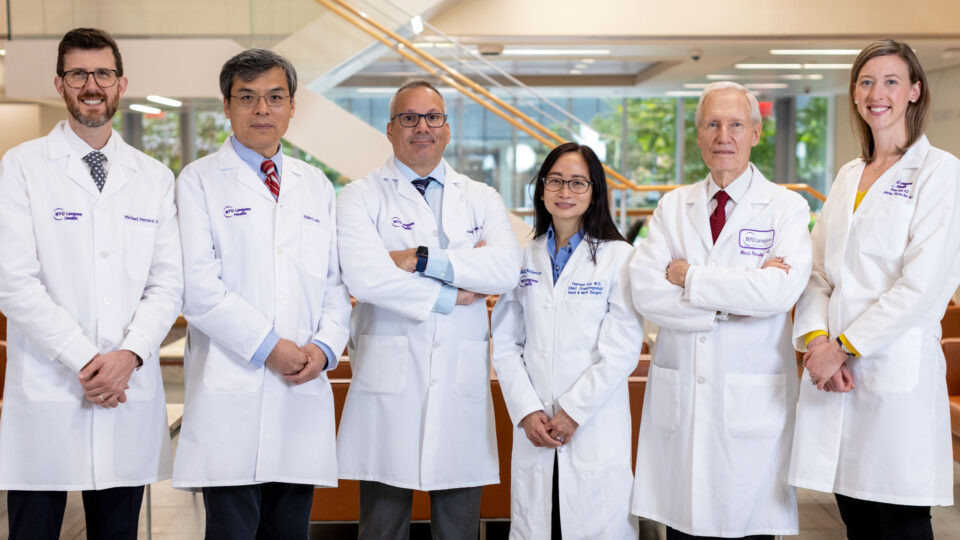
“Our experts treat more over 600 patients each year using SRS, making NYU Langone one of the highest volume centers in the United States,” says Joshua Silverman, MD, PhD, an associate professor radiation oncology and neurosurgery who specializes in brain cancer.
As few prior studies using SRS had included patients with larger numbers of brain metastases, Dr. Silverman and colleagues including Douglas Kondziolka, MD, a professor of radiation oncology and neurosurgery, have undertaken several studies evaluating the use of Gamma Knife SRS in patients with ≥25 brain metastases—a population traditionally associated with poor prognosis.
“For patients with multiple brain metastases, particularly in subsets that can be treated successfully with immunotherapy, or molecular targeted agents, these patients can often live for years.”
Joshua Silverman, MD, PhD
Hippocampal Sparing with SRS
In a recent dosimetric analysis of prospective registry data, they identified 89 patients treated with SRS for ≥25 brain metastases in single or multiple sessions. They analyzed the distribution of metastases relative to the hippocampal avoidance (HA)-region and hippocampi (HC), and measured the incidence of perihippocampal tumor location. Doses from each session were summed to calculate HC dose.
Among the 89 patients, the median number of tumors irradiated per patient was 33 (range 25-116), delivered in a median of 3 (range 1-12) sessions.
HC doses were significantly correlated with the tumor number and volume. Of 3,059 total treated tumors, 83 (2.7 percent) were located in the HA-region, affecting 57 percent of patients. The researchers also reported that 38 tumors (1.2 percent) abutted or involved the HC itself.
“There may be improvement in neurocognitive outcomes with hippocampal sparing using SRS rather than hippocampal avoidance whole brain radiotherapy (WBRT) techniques,” Dr. Silverman says. “Patients who receive WBRT often experience neurocognitive side effects, including short term memory loss and deficits in expressive language skills, shortly after treatment—SRS affords hippocampal sparing.”
Prolonging Survival for Patients with Brain Metastases
Dr. Silverman notes given more patients and brain metastases are being treated with SRS alone, it is important to understand how patient, tumor, and treatment factors affect functional status and overall survival.
In a second study, the researchers examined survival outcomes and dosimetry to critical structures in 95 patients treated with Gamma Knife SRS for ≥25 metastases.
They reported the median number of SRS sessions per patient was 3 (range 1-12), with nearly all patients (98%) having more than one session. On univariate analysis, factors significantly affecting overall survival included histology, tumor volume, tumor number, diagnosis-specific graded prognostic assessment, brain metastasis velocity, and need for subsequent WBRT. Results showed that in selected patients with a large number of cumulative brain metastases, multiple courses of SRS are feasible and safe.
“Together with new systemic therapies, we observed survival rates that compare favorably to larger contemporary cohorts, while avoiding WBRT in most patients,” Dr. Silverman says. “Our findings support SRS as a standard practice in selected patients with larger numbers of brain metastases.”