Scott M. Rickert, MD, is chief of the Division of Pediatric Otolaryngology and a co-director of the Pediatric Aerodigestive Center. Also an associate professor of otolaryngology, pediatrics, and plastic surgery, his subspecialty interests include conditions affecting the pediatric airway, voice, and swallowing.
Dr. Rickert was recently elected president of the Aerodigestive Society, a multidisciplinary group committed to advancing research, clinical care, and public health for patients with complex aerodigestive disease. Here, he discusses emerging topics in diagnosis and treatment, and the rewards and challenges of treating children with highly complex cases.
Physician Focus: The Aerodigestive Center treats patients with a combination of multiple and interrelated airway conditions. As an otolaryngologist, what drew you to treating these complex pediatric cases?
Dr. Rickert: I came to pediatric otolaryngology prepared to be involved in all procedures but became focused on the aerodigestive kids because they’re some of the patients that need the most help. They are often undertreated and kept at their baseline without comprehensive care. They’re also among the most interesting patients to me.
A lot of these kids have chronic conditions, so you have long-lasting relationships with them. We see many of our patients become young adults. Helping them thrive not only impacts their lives, but it has a big impact on their families and their families’ lives.
Coordinating Complex Care
Physician Focus: Aerodigestive care is, by definition, a multispecialty model. What are some of the benefits and challenges of this in day-to-day medical practice?
Dr. Rickert: Aerodigestive cases require close coordination. Some of these patients are just airway patients and some are primarily GI. The multiple areas of concern allow for cross-pollination of ideas and collaboration. Eighty percent of these patients have need for a speech or voice therapist, so it’s a great benefit to have that perspective.
Our team holds weekly care meetings in the ENT office, where all our equipment is located. Despite a potential financial challenge to maintaining a central location—how can you have four doctors in one place when you could have them in different offices?—when you evaluate the model and all the care these patients get, it’s actually quite efficient to have all the doctors together. And it’s better for the kids and their families.
Learning from Other Programs
Physician Focus: You’ve just been elected president of the Aerodigestive Society. What are some of your objectives for that group?
Dr. Rickert: The society started out about 10 years ago to integrate all the different programs in the United States for sharing information, conducting multi-institutional research, and establishing care guidelines.
“I’ve been trying to encourage everyone around the country to promote multidisciplinary care at their institutions, and if that’s not possible, to look to their community or to others across the country who can support them.”
Scott M. Rickert, MD
As president, I’ve been trying to encourage everyone around the country to promote multidisciplinary care at their institutions, and if that’s not possible, to look to their community or to others across the country who can support them.
For instance, one hospital may not have pediatric GI, but they may collaborate with another hospital in their area that does. We have a great perspective on how to build a team here in New York with our large volume, but it’s interesting to see how people in Cincinnati, or Argentina, are modeling aerodigestive care.
Always, when you have complex cases, it’s helpful to talk with other people who treat similar cases to see whether their approaches are different or better. COVID-19 has had many implications for patients who need complex care. We’ve been trying to keep aerodigestive care in the forefront.
Imaging Airway Dynamics
Physician Focus: Are there any new equipment or therapeutic innovations on the horizon?
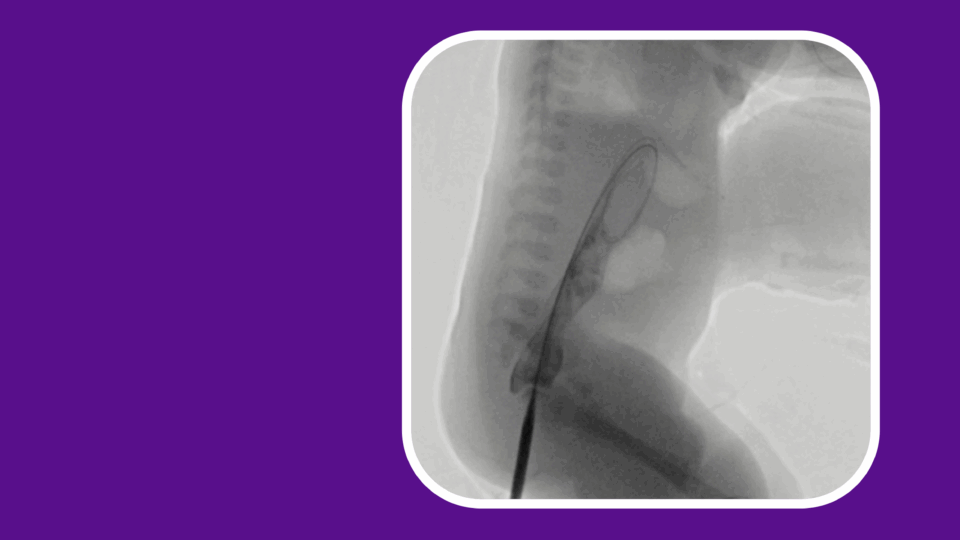
Dr. Rickert: We’ve already been using cutting-edge imaging to understand what’s going on in the lungs and video swallow tests to confirm what a speech/language pathologist is seeing. Today, we are doing sleep endoscopies because a lot of these kids have sleep and breathing problems. It’s a new, innovative technique to understand what their airway does when they’re sleeping.
We are developing simulation software to understand flow dynamics in the airway, not only in breathing, but also swallowing. Plus, we are creating 3D models of the airway using 3D printing. This allows us to plan out a surgery virtually so when we’re doing it in real life, we can be more efficient.
We’re in the planning stages of some studies to better understand cough. And of course, we’re always striving to innovate care in prescribing medicines for those kids who have chronic issues.
Rewards of Collaboration
Physician Focus: What would you say to get a medical trainee interested in this field?
Dr. Rickert: It’s a wonderful place to be because of the collaborative nature of the work. We’re sharing all the time. If you want to be involved, whether you’re a pulmonologist, a GI specialist, or an ENT, there’s a small dynamic group that’s always looking forward. Not only does this impact your patients, but anything that’s being done locally impacts kids across the country.
This is what you go into medicine for—to make a difference in people’s lives!