When a 25-year-old female was diagnosed with proliferative vitreoretinopathy (PVR) total retinal detachment in the right eye—deemed inoperable by two retinal specialists in 2024—her NYU Langone Health care team thought otherwise, setting their sights on restoring her vision and functional independence.
The patient was referred to leading uveitis specialist C. Michael Samson, MD, MBA for evaluation of panuveitis in her right eye. She had a complex ocular and medical history, including no vision in her left eye since childhood, congenital cataract, and pregnancy complications.
While pregnant, the patient had discontinued immunosuppressive therapy, leading to uncontrolled inflammation and near complete vision loss in her right eye.
Dr. Samson reasoned that she had PVR retinal detachment with inflammation secondary to uveitis. Retinal detachment, while known in patients with uveitis, affects less than 5 percent of eyes with active inflammation seen at tertiary referral centers.
“She had poor vision for her entire life and could only see out of her right eye since childhood,” Dr. Samson explains. “Prior to seeing her, she was treated for uveitis at another institution.”
“She couldn’t see anything—only light and dark in her right eye. She had never seen her newborn baby.”
C. Michael Samson, MD, MBA
After successfully managing the inflammation with systemic adalimumab, Dr. Samson referred her to Kenneth Wald, MD, director of vitreoretinal surgery and retinal disease, who evaluated her for a potential vitrectomy to restore vision in her right eye.
“She couldn’t see anything—only light and dark in her right eye,” Dr. Samson says. “Her mother had to help her in and out of the consult room, and she had never seen her newborn baby.”
A Difficult Case for Surgery
Determining whether the patient was operable was the most challenging part of the case, notes Dr. Wald, given the patient’s poor surgical history.
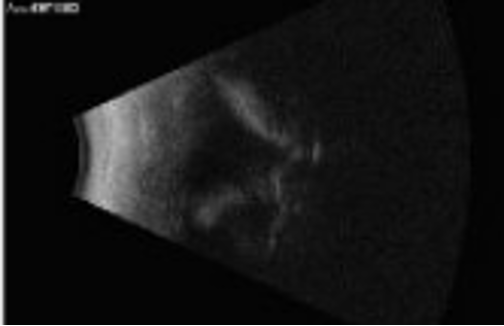
After performing an ocular ultrasound, Dr. Wald anticipated that at least some degree of vision improvement was possible. He recalls uncertainty however, as the posterior segment view of the right eye was limited due to significant corneal fibrosis, as well as fibrosis over the intraocular lens.
Ultimately, Dr. Wald and his team recommended vitrectomy surgery. “This was one of the worst cases of retinal detachment I had ever seen,” recalls Dr. Wald. “But based on our long experience in the procedure, I knew we had shot at achieving success.”
“Based on our long experience in the procedure, I knew we had shot at achieving success.”
Kenneth Wald, MD
The surgical team employed a traditional method of vitrectomy with membrane peel, endolaser, and silicone oil tamponade in the right eye. The patient was discharged and went home soon after the procedure.
Remarkable Improvement
In the weeks that followed, the patient’s vision began to incrementally improve—eventually reaching 20/350, Dr. Wald says. She is now able to complete normal activities like traveling on the subway and caring for her child, he added.
“She had the opportunity to see her newborn baby for the first time,” Dr. Wald says.
While her vision is not perfect, Dr. Wald explains that it will likely remain stable over time. For similar cases, he encourages providers to refer patients to institutions with deep expertise in vitreoretinal procedures, while also highlighting the critical role of systemic immunosuppression in uveitis management.







