A Rare Congenital Heart Defect
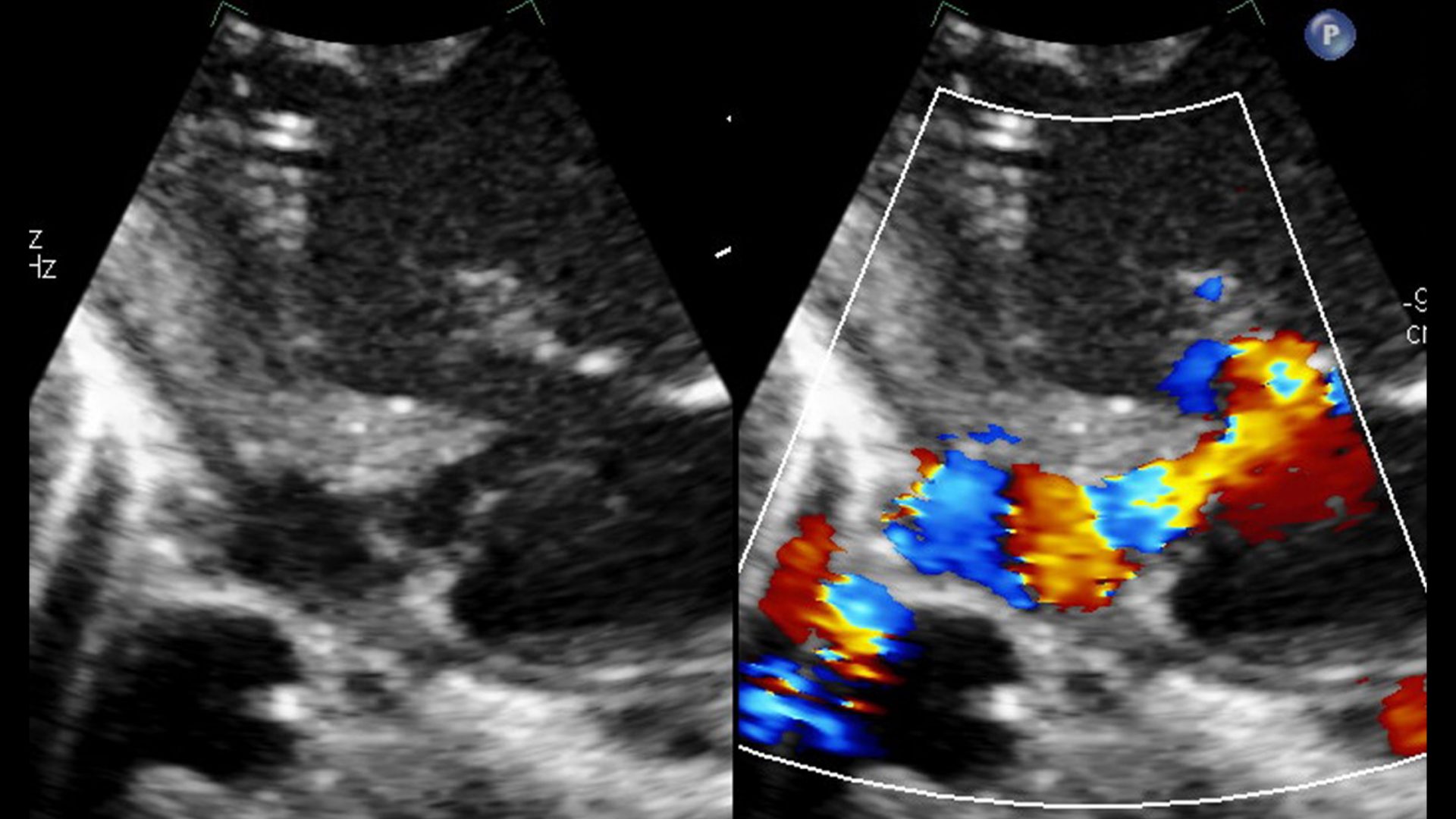
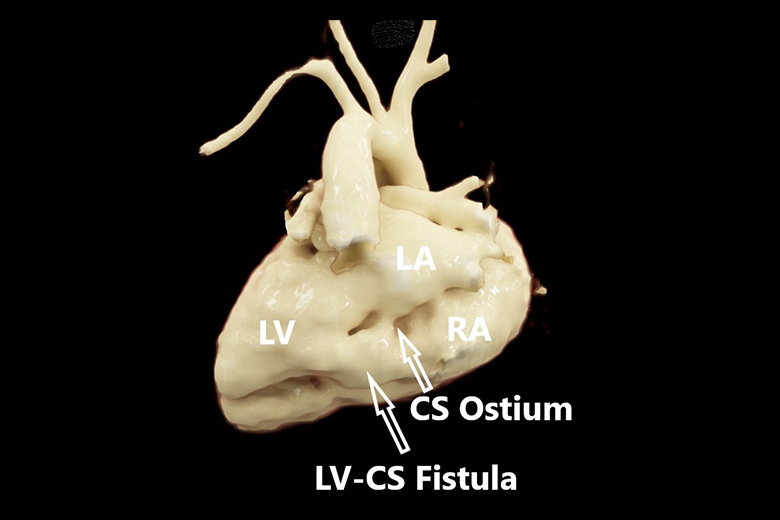
Congenital left ventricle (LV) to coronary sinus (CS) fistula is a rare entity that can occur either in isolation or in conjunction with other heart defects. With only six prior case reports in the literature, a carefully planned intervention leveraging advanced catheter techniques and intraprocedural imaging is needed to ensure optimal outcomes.
In September 2019, when a young male infant was delivered at term to a 34-year mother, cardiac imaging revealed the congenital LV to CS fistula. In addition to the shunt from the fistula, there was another problem.
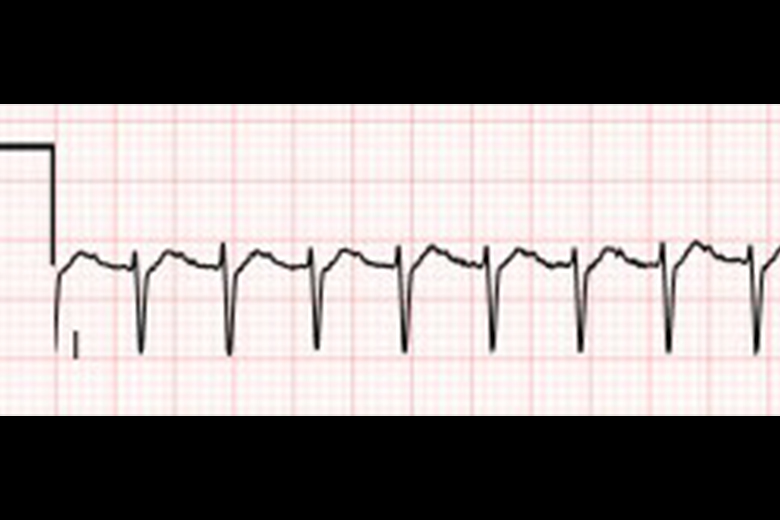
“The baseline electrocardiogram findings were notable for a Wolff-Parkinson-White pattern,” explains Frank Cecchin, MD, the Andrall E. Pearson Professor of Pediatric Cardiology and director of the Division of Pediatric Cardiology at NYU Langone Health. “This is the first case report that describes an association of the LV-CS fistula with Wolff-Parkinson-White syndrome.”
“This is the first case report that describes an association of the LV-CS fistula with Wolff-Parkinson-White syndrome.”
Frank Cecchin, MD
Postnatally, refractory supraventricular tachycardia consistent with Wolff-Parkinson-White syndrome required therapy with several anti-arrhythmic drugs.
A Very Challenging Procedure
After discussions among the care team, it was apparent that surgical intervention posed unacceptable risk, as the high-pressure thin-wall fistulous connection located deep and posteriorly behind the heart would be nearly impossible to access surgically.
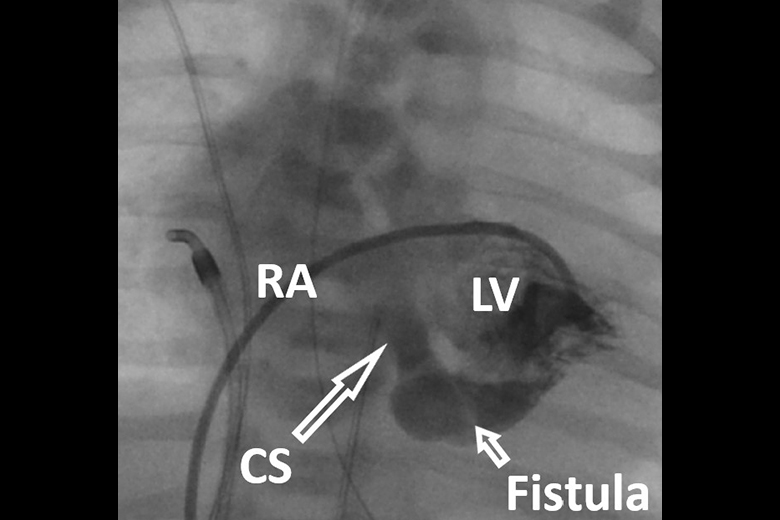
“We all agreed that a percutaneous approach would be preferable,” notes interventional cardiologist Michael Argilla, MD, director of the Pediatric Catheterization Laboratory. When signs of high-volume heart failure emerged, Dr. Argilla and his partner, pediatric interventional cardiologist Sunil Saharan, MD, made the decision to intervene early, but the risks were high.
The challenge with infants is their small vessels and heart chambers, which limits the size and manipulation of catheters, adds Dr. Argilla. For this procedure, there was a need to avoid implanting a device that would obstruct future routes to the accessory pathway during a subsequent electrophysiology ablation, performed by Dr. Cecchin.
The end result was a marathon catheterization, which involved the surgical team attempting three different approaches to closing the fistula before successfully implanting the device.
A Successful Recovery
Remarkably, following the successful catheter device closure of the LV to CS fistula on day 12 of life, the patient later underwent successful ablation of the accessory pathway.
“This was the most challenging procedure we’ve done—and we’re very happy to report an excellent post-procedural result,” says Dr. Argilla, “Two years later, when we met Max again, he presented as a healthy and energetic toddler.”
“This was the most challenging procedure we’ve done—and we’re very happy to report an excellent post-procedural result.”
Michael Argilla, MD