A team of neurologists at NYU Langone Health has crafted a first-of-its-kind training program to instruct neurology residents in performing virtual exams. The unique program includes a simulation component, enabling trainees to rehearse with an actor portraying a patient they will likely see in clinical practice.
“Our curriculum provides much-needed opportunities for future neurologists to hone their telemedicine skills, which will become increasingly important as the field evolves,” says Arielle M. Kurzweil, MD, an associate professor of neurology and director of NYU Grossman School of Medicine’s Neurology Residency.
“Our curriculum provides much-needed opportunities for future neurologists to hone their telemedicine skills.”
Arielle M. Kurzweil, MD
Since its launch in 2020, the three-year teleneurology program has educated at least 68 neurology residents. A recent study in Neurology: Education details the program’s effectiveness and discusses strategies for adjusting hands-on examination methods for virtual settings.
Adapting to the Virtual Setting
While virtual healthcare technology has existed in some form for decades, physicians still receive little formal training in its use.
“There are some suggested guidelines for teaching teleneurology, though no standard approach among programs,” says Dr. Kurzweil, who served as senior author on the new study. “This is a new frontier. We’re learning alongside trainees what will ensure the best outcomes for learners and patients.”
The researchers found that neurology residents preferred various methods for teleneurology training, such as didactics with slides, live demonstrations, simulated experiences, and starting with live patients to reading materials or articles.
Simulation Cements Proper Techniques
Unlike many other training courses that emphasize telehealth communication skills, the NYU Grossman School of Medicine curriculum’s unique simulation component features a virtual exam. In these 10-minute sessions, residents are expected to diagnose their “patients” and discuss a treatment plan.
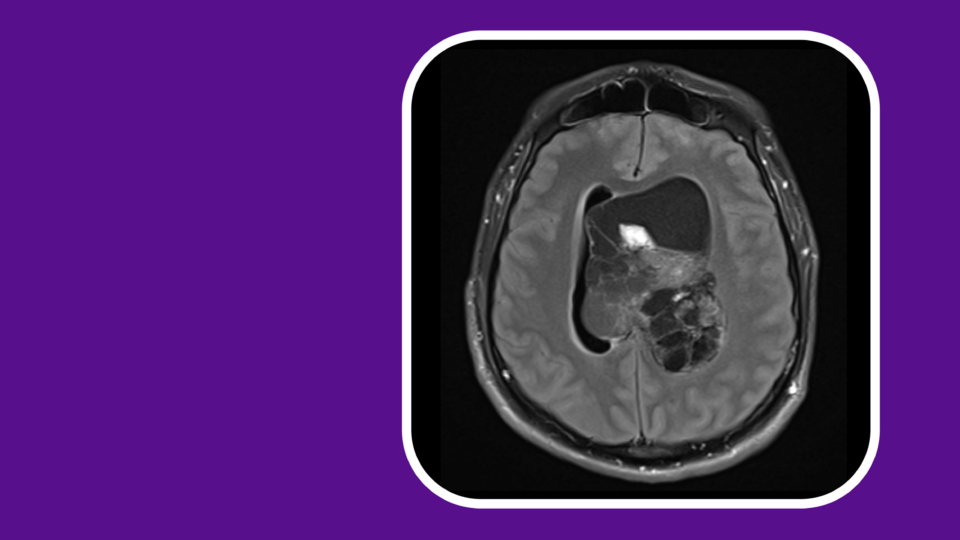
Actors play “patients,” mimicking the symptoms of meralgia paresthetica, which results from injury to a nerve.
“Since we often see patients with meralgia paresthetica, which is commonly misdiagnosed, we decided this was a practical teaching opportunity for virtual exams,” says study co-author Neil A. Busis, MD, a clinical professor of neurology who also serves as director of the telehealth program in neurology. “It’s also much easier for actors to portray sensory loss than to accurately replicate motor loss found with other conditions.”
“Instructing patients to perform a self-assessment requires excellent verbal communication and creativity—if you don’t have the conventional in-office tools, what’s a reasonable workaround?”
Neil A. Busis, MD
During the simulated exam, trainees are graded on hard skills such as accuracy and thoroughness. Soft skills, or “webside manner,” like maintaining eye contact, are also evaluated as these behaviors, the authors say, can be lost during the shift from in-person exams to remote ones.
Additionally, trainees are required to guide the on-screen “patient” in adjusting their camera so their whole body is visible, and in resolving basic technical issues like unmuting. “Overcoming challenges like poor lighting in the patient’s home, which are realities in daily practice that can limit our ability to evaluate the patient accurately, are an essential skill,” says Dr. Busis.
Since the trainees cannot touch the patients in a virtual encounter, Dr. Busis stressed how they must be able to coach patients to conduct self-assessments. “Instructing patients to perform a self-assessment requires excellent verbal communication and creativity—if you don’t have the conventional in-office tools, what’s a reasonable workaround?”
Curriculum Increases Comfort with Virtual Exams
The new report surveyed trainees with no prior education in virtual care and no previous experience with teleneurology before the program. The authors found that comfort with virtual exams improved from an average score of 2.8 out of 5 (5 representing maximum confidence) to 3.8 out of 5 after the first year.
Interest in telehealth grew as well, increasing from an average score of 3.5 out of 5 (5 representing the highest interest) to 4.3 out of 5.
The Future of Teleneurology Training
Telehealth has become an integral part of medical practice, particularly in neurology clinics where a blend of in-person and remote encounters are emerging as the standard for routine care. According to a recent report from Dr. Kurzweil, Dr. Busis, and colleagues, both patients and neurologists agree that the vast majority—over 90 percent—of teleneurology encounters are effective.
Multimodal learning with a simulation component appears to be the key to success in teleneurology training. The team, alongside other colleagues, has added a telestroke simulation to the curriculum for senior residents and may also incorporate new neurologic symptoms like headache, weakness, and dizziness into the simulated encounters.