This past June, the Institut de France co-awarded its Grand Prize in Science (Grand Prix scientifique) to Kathryn J. Moore, PhD, director of NYU Langone Health’s Cardiovascular Research Center. The award—the largest of its kind in cardiovascular research—honored Dr. Moore for her pioneering research on how the innate immune system recognizes excess cholesterol in the body and responds by inducing the chronic inflammation that drives atherosclerosis.
Here, Dr. Moore reflects on the prestigious prize, her groundbreaking discoveries that led to it, and what excites her about the future of cardiovascular research.
Physician Focus: Dr. Moore, what have you learned about how macrophages can trigger the kind of chronic inflammation that drives atherosclerosis?
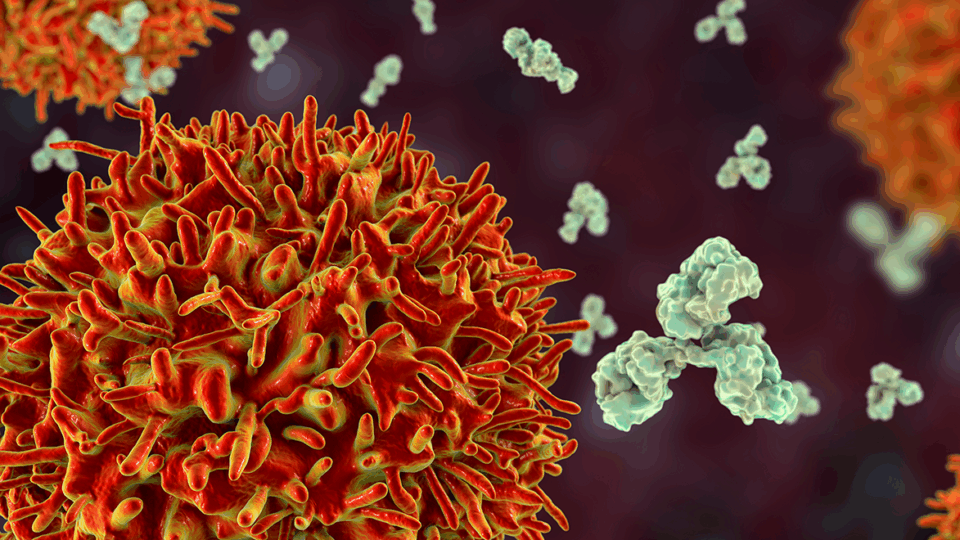
Dr. Moore: In atherosclerosis, macrophages enter the artery wall to clear low-density lipoproteins (LDL) that accumulate due to hypercholesterolemia. But once the macrophages ingest the LDL, they can become overloaded with cholesterol and trapped in the vessel wall—a good deed gone bad. The accumulating macrophages call in more immune cells to help resolve the issue, but this backfires, forming chronic inflammation. It’s that chronic, low-grade inflammation that drives plaque formation in the arteries over decades, leading to atherosclerosis.
“Once the macrophages ingest the LDL, they can become overloaded with cholesterol and trapped in the vessel wall—a good deed gone bad.”
Kathryn J. Moore, PhD
My work focuses on trying to understand what makes beneficial inflammation turn chronic, what the key pathways are, and whether we can reverse them. The Grand Prix scientifique was awarded specifically for my discovery of how macrophages recognize LDL, which is by using the same receptors designed to detect and defend against pathogens. By engaging these defense receptors, LDL triggers the production of potent pro-inflammatory molecules and inflammation.
Physician Focus: What about your work on RNA molecules—how are they involved in cholesterol metabolism and inflammation?
Dr. Moore: My lab discovered that microRNAs can repress the expression of genes required for the macrophage to rid itself of the excess cholesterol. By targeting these microRNAs, we enhanced cholesterol efflux from the macrophages, which allowed the cells to leave the artery wall and reduced inflammation in the plaque.

I’m also really interested in long non-coding RNAs, many of which are not conserved between humans and preclinical animal models. For years, drug development was based on studies in animal models. But when the drugs were tested in humans, researchers found different results or they didn’t pan out. Understanding that there can be a layer of transcriptional control or genome organization in humans that is not conserved in other animals can offer tremendous insights. For the last 10 years, my lab has been studying how these human-specific long non-coding RNAs regulate biological processes, whether it’s cholesterol metabolism or inflammation in atherosclerosis.
Physician Focus: What are you most excited about in inflammation-related research, and what do you want to tackle next?
Dr. Moore: Over the past five years, we’ve seen a revolution in the technologies available to us for research. We are now able to look at tissues at the single-cell level and use techniques like spatial transcriptomics to map cellular gene expression within tissue. It’s giving us unprecedented insight into the complexity of the tissues and the interactions between different cell types within them.
For our work on inflammation in the plaque, we are using these technologies to interrogate unique cell types to understand the ones that contribute to plaque progression versus those types that contribute to regression. We want to know how cells are communicating in these different states, and we’re looking at gene expression profiles between the cells to understand what that communication might look like.
Physician Focus: What do you see as the next challenge to further improving treatments for cardiovascular disease?
Dr. Moore: Lipid-lowering therapies have been highly successful at reducing cardiovascular risk, but many patients still go on to have a heart attack. Even people whose LDL has been lowered very dramatically continue to be at risk of having a cardiac event.
“We need complementary therapies to lipid-lowering, and targeting inflammation in the plaque is one area that’s thought to hold promise.”
Because of this, we need complementary therapies to lipid-lowering, and targeting inflammation in the plaque is one area that’s thought to hold promise. We seek to develop novel therapies that can convert chronic inflammation into self-resolving inflammation by targeting pathways that hinder its resolution.
Physician Focus: Finally, what does it mean for you to earn this prestigious award?
Dr. Moore: It’s a tremendous honor to receive this prize, which celebrates the outstanding contributions to cardiovascular research that have been made by luminaries in my field. I have truly flourished in the collaborative and supportive environment at NYU Langone. It has taken my science to a different level. I’ve also been very lucky to work with many talented postdocs and graduate students. Really, this award recognizes the entire lab, past and present. I would not have made these discoveries without my incredible team.