Case Highlights:
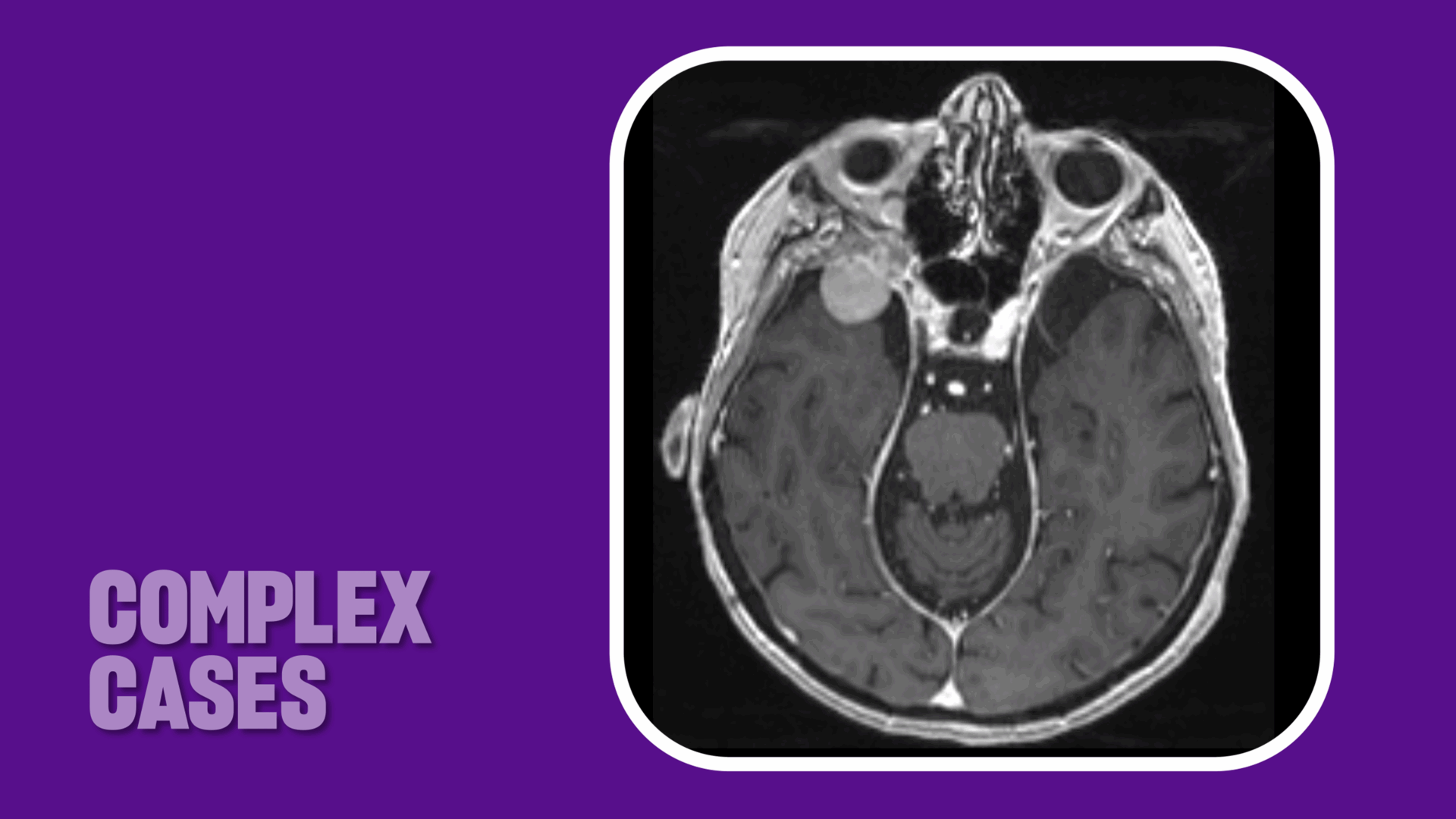
- The tumor extended from the orbit and orbital apex into the middle cranial fossa, approaching the cavernous sinuses and compressing the optic nerve; the frontal and ethmoid sinuses were pneumatized.
- TONES with lateral orbitotomy allowed safe access while minimizing the risk of sinus violation and CSF leak.
- The patient’s vision was restored significantly after surgery and continues to improve.
In the fall of 2025, a female in her 80s with significant vision loss in her right eye was referred by her ophthalmologist to the emergency department at NYU Langone Health. The patient had previously undergone resection of a posterior fossa meningioma and was being monitored for a second meningioma in the spheno-orbital region; it had been several years since her last imaging follow-up. Aside from vision loss, she was in otherwise good health.
“Radiographic imaging revealed that the spheno-orbital meningioma had grown significantly, causing compression of the optic nerve,” says neurosurgeon Donato R. Pacione, MD, attending physician on the case. “The tumor was extending from the orbit and the orbital apex into the middle cranial fossa and intracranial space. It was up against the anterior temporal pole, with a tail at the level of the cavernous sinus.”
Other notable features included markedly pneumatized frontal and ethmoid sinuses that extended over the orbit and tracked along the proximal orbital roof, nearly reaching the level of the sphenoid wing.
Given these constraints, transorbital neuroendoscopic surgery (TONES) was determined to offer the best access to orbital and intracranial compartments compared to traditional transcranial or suborbital approaches, while minimizing the risk of CSF leak and other potential complications.
Specialists at NYU Langone’s Skull Base Surgery Center are leaders in advanced minimally invasive surgical techniques, including TONES for tumors affecting the brain and skull base. “Seeing that the patient’s tumor fell within the limits of what could be safely resected transorbitally—and that this approach would avoid the risk of puncturing the sinuses—clinched it as our surgical strategy,” Dr. Pacione says.
Complex Skull-Base Surgical Expertise
“When treating spheno-orbital meningiomas and other skull-base tumors, expertise across all relevant surgical approaches is critical,” Dr. Pacione says. In this case, working alongside him was oculoplastic surgeon, Stella Chung, MD. After performing an incision at the level of the superior eyelid crease, Dr. Chung opened the orbit, delicately elevated the globe and periorbital tissues from the lateral orbital wall, and removed the trigone of the sphenoid.
“Orbital surgeons play a useful role in TONES because we already perform this technique for patients with thyroid eye disease to provide orbital decompression,” Dr. Chung says. “Orbital surgery is a tight space. My primary concerns are maintaining hemostasis and minimizing pressure on the eye to prevent vasospasm or ischemia, while also avoiding injury to the extraocular muscles.”
“Orbital surgeons play a useful role in TONES surgery because we already perform this technique for patients with thyroid eye disease.”
Stella Chung, MD
Using a micro endoscope and high-speed diamond drill, Dr. Pacione then created a small window in the orbital rim. He removed a section of the lateral orbital wall without disconnecting it from the muscle to allow for better healing and more natural postsurgical alignment while avoiding the need for cranial plating.
After gaining access to the intraorbital tumor, Dr. Pacione used neuro-navigation to visualize, coagulate, debulk, and detach the meningioma from surrounding structures. “We were able to completely remove the tumor without disturbing the brain,” Dr. Pacione says. When all excisable tumor tissue was safely removed, he reconstructed the orbit with a synthetic dural repair substitute and sutured the orbit in place around the lateral orbital rim.
Postoperative Management
With resection of the 2.5 cm grade 1 meningioma, the four-hour surgery resulted in fully decompressing the optic nerve. Postoperatively, vision in the patient’s right eye significantly improved by the following day.
“Her vision should not be at risk again in the future.”
Donato R. Pacione, MD
The patient went home on day two and her vision has steadily improved since surgery. She will continue to be monitored with periodic MRIs. “Surgery was effectively a cure for her. Her vision should not be at risk again in the future,” Dr. Pacione says.