A toddler with end-stage liver disease secondary to Alagille syndrome experienced a smooth recovery after surgeons at NYU Langone Health teamed up to perform a successful split liver transplant.
The 2-year-old patient was referred to the Pediatric Liver Disease and Transplant Program at Hassenfeld Children’s Hospital for evaluation by Adam Griesemer, MD, and Alejandro Torres-Hernandez, MD, attending surgeons on the case. “The patient’s recovery has been remarkable,” says Dr. Griesemer. “His quality of life has improved far sooner than would have been expected, and he remains playful and full of energy.”
Nadia Ovchinsky, MD, director of the Division of Pediatric Gastroenterology and Hepatology, had been following this transplant patient since infancy. Alagille syndrome, an autosomal dominant disorder that carries a mortality rate of up to 10 percent, runs in his family.
“The degree of his liver disease, intractable itching, and severe failure to thrive were clear indicators that a liver transplant was needed.”
Nadia Ovchinsky, MD
“Liver transplant was a challenging decision for this family,” says Dr. Ovchinsky. “However, the degree of his liver disease, intractable itching, and severe failure to thrive were clear indicators that a liver transplant was needed.”
Success Despite Risks
The team anticipated an elevated risk of transplant-related complications due to the complex presentation of Alagille syndrome and the patient’s poor nutritional status. Despite months of aggressive supplementation, the patient consistently remained well below the first percentile for both height and weight.
In addition to significant failure to thrive, he had renal tubular acidosis, pulmonary artery stenosis, fat-soluble vitamin deficiencies, and severe intractable pruritis.
“Our team is well known for successfully executing these complicated procedures.”
Alejandro Torres-Hernandez, MD
“We had a thorough discussion with the patient’s family, addressing the specific risks related to the split liver transplant and the potential advantages,” says Dr. Torres-Hernandez. “Our team is well known for successfully executing these complicated procedures.”
The Split Liver Transplant
After the patient was listed for transplantation, the team waited for the first appropriate organ offer.
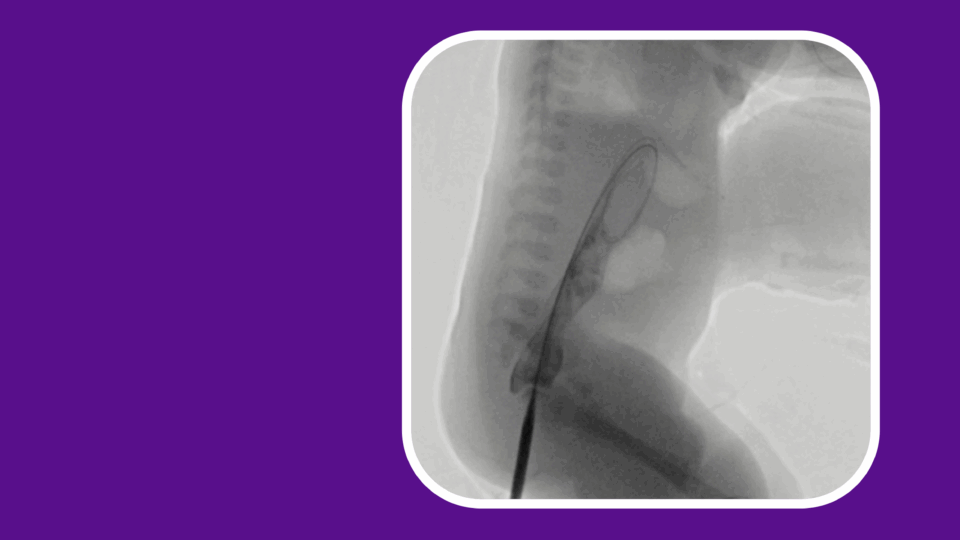
Within a month, the patient was offered a healthy adult liver for transplant. The organ would be too big for the recipient unless it was split into two, allowing both halves to be used for two different patients. For the pediatric recipient, the split graft was a left lateral lobe with a single left hepatic vein. For the adult patient, the split graft was the right lobe.
“About 50 percent of liver transplants performed on children under the age of eight involve splitting a deceased donor’s liver,” Dr. Griesemer adds. “Split liver transplantation is an effective strategy to reduce the donor organ shortage and waitlist mortality, especially for pediatric patients.”
During the surgery, the patient’s liver was completely removed. The left lateral segment graft was then transplanted to the recipient. “The size of the donor’s left lateral segment was almost exactly the same size as a normal liver for the age of the recipient,” says Dr. Griesemer.
A Flawless Procedure
After restoring blood flow to the transplant, the liver had excellent perfusion and immediately started to function well. According to Dr. Griesemer, the procedure’s success can be attributed to the collaboration and hard work of multiple team members, including surgeons, anesthesiologists, surgical assistants, scrub nurses, and leaders outside of the operating room.
“The procedure was executed flawlessly,” says Dr. Griesemer. “Going in, we were confident in our team’s approach, and we planned this well.”
“Going in, we were confident in our team’s approach, and we planned this well.”
Adam Griesemer, MD
Nine months after surgery, the patient’s recovery has been excellent, marked by consistent improvements in clinical and functional measures. “The patient’s quality of life has returned to normal, and he is meeting developmental milestones as expected,” says Dr. Ovchinsky.
In the coming months, NYU Langone will launch a new program to improve care for those with Alagille syndrome, offering specialized support for both pediatric and adult patients. Dr. Ovchinsky, who will lead the initiative, explains that specialized care will include experts in hepatology, surgery, nephrology, and cardiology.