Referral Notes:
- An NYU Langone Health analysis found that after PCI in patients with diabetes, ticagrelor-based DAPT was linked to a 16.57 percent rate of composite heart attack, stroke, bleeding complications, and death compared to 14.23 percent for prasugrel-based DAPT.
- Worse outcomes with ticagrelor were seen in patients with diabetes for less than five years and in those with a high risk of bleeding.
- The results suggest the two medications should not be used interchangeably.
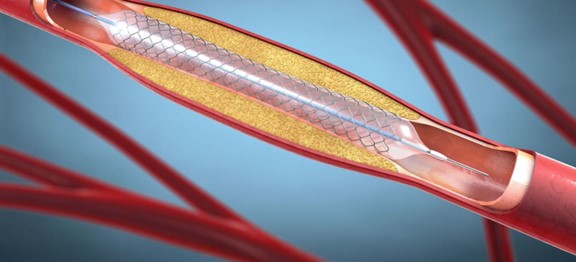
One year of treatment with either ticagrelor or prasugrel by patients with diabetes after percutaneous coronary intervention (PCI) did not provide the same level of protection against stent clotting, heart attacks, and bleeding complications, according to findings from the TUXEDO-2 study presented at the American Heart Association’s Scientific Sessions 2025.
“Our results suggest that prasugrel may be the better choice for patients with type 1 or type 2 diabetes,” says study lead author and co-chair of the trial Sripal Bangalore, MD, director of the Cardiovascular Outcomes Group at NYU Langone Health and in the Leon H. Charney Division of Cardiology.
“Our results suggest that prasugrel may be the better choice for patients with type 1 or type 2 diabetes.”
Sripal Bangalore, MD
“The results were unexpected, as we initially hypothesized that ticagrelor would be equally effective, if not better, than prasugrel,” Dr. Bangalore adds. “These findings highlight the importance of selecting the right medication, as our data indicate that ticagrelor and prasugrel are not interchangeable.”
TUXEDO-2
The TUXEDO-2 study is a randomized clinical trial to evaluate strategies for treating coronary artery disease in patients with diabetes. Participants include 1,800 adults in India with type 1 or type 2 diabetes and multivessel coronary disease who underwent PCI with a drug-eluting stent.
The primary clinical trial is comparing the safety and efficacy of two drug-eluting stents for PCI in patients with diabetes and multivessel disease. The objective of this analysis was a randomized comparison of a ticagrelor- versus prasugrel-based dual antiplatelet therapy (DAPT) to assess potential impact on heart attack, stroke, major bleeding, and death.
According to the “2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients With Acute Coronary Syndromes,” continued DAPT with aspirin and a P2Y12 inhibitor (such as ticagrelor or prasugrel) is recommended for at least one year for all patients who receive a drug-eluting stent.
Ticagrelor vs. Prasugrel
The primary combined outcome of heart attack, stroke, bleeding complications, and death occurred at a rate of 16.57 percent in patients taking ticagrelor compared to 14.23 percent in those taking prasugrel.
When evaluated by outcome, nonfatal heart attack occurred in 5.96 percent of the ticagrelor group versus 5.21 percent of the prasugrel group; major bleeding occurred in 8.41 percent of the ticagrelor group versus 7.14 percent of the prasugrel group; and death was reported for 5.03 percent of the ticagrelor group versus 3.67 percent of the prasugrel group.
Worse outcomes were observed with ticagrelor in patients with diabetes duration of less than five years (a 63 percent higher risk) and in those with a high risk of bleeding (a 61 percent higher risk).
“These medications are often considered interchangeable, but our findings suggest important differences.”
“These medications are often considered interchangeable, but our findings suggest important differences,” says Dr. Bangalore. “For individuals with diabetes and complex coronary disease, prasugrel may offer distinct advantages over ticagrelor.”
Further Studies
The trial is ongoing and will continue to follow these patients for approximately five years after stent implantation.
Study limitations included that both patients and physicians were aware of the assigned medications, which could introduce bias. Additionally, treatment compliance was not monitored, so it’s unclear whether participants consistently took their medications as prescribed.