NYU Langone Health recently completed a merger with the former Long Island Community Hospital, now named NYU Langone Hospital—Suffolk. With that merger came a meticulous audit and a host of institutional changes.
For orthopedic services and care, the integration has been a massive success, with several key quality metrics improving in a relatively short period of time.
Under the guidance of Joseph Bosco III, MD, vice chair of clinical affairs and director of quality and patient safety in the Department of Orthopedic Surgery, and Claudette M. Lajam, MD, chief safety officer in the department, acclaimed orthopedic surgeons James D. Capozzi, MD, and Richard Savino, MD, were charged with bringing many of the tried and tested best practices from the Manhattan campus to Suffolk. Their goal is to ensure patients receive the highest quality care close to home and reflects the longstanding vision of department chair Joseph D. Zuckerman, MD, who set the initiative in motion to bring the same high standards of care to every location.
Here, Drs. Capozzi, Lajam, and Savino share some of these best practices, and tell the story of how they successfully revitalized an orthopedics department that had been facing significant challenges.
Physician Focus: After the merger and audit, what metrics concerned you most?
Dr. Savino: The complication rates were alarmingly high—and we didn’t know why. As a leadership team, our first step was to figure out why, then devise a strategy to bring the numbers down.
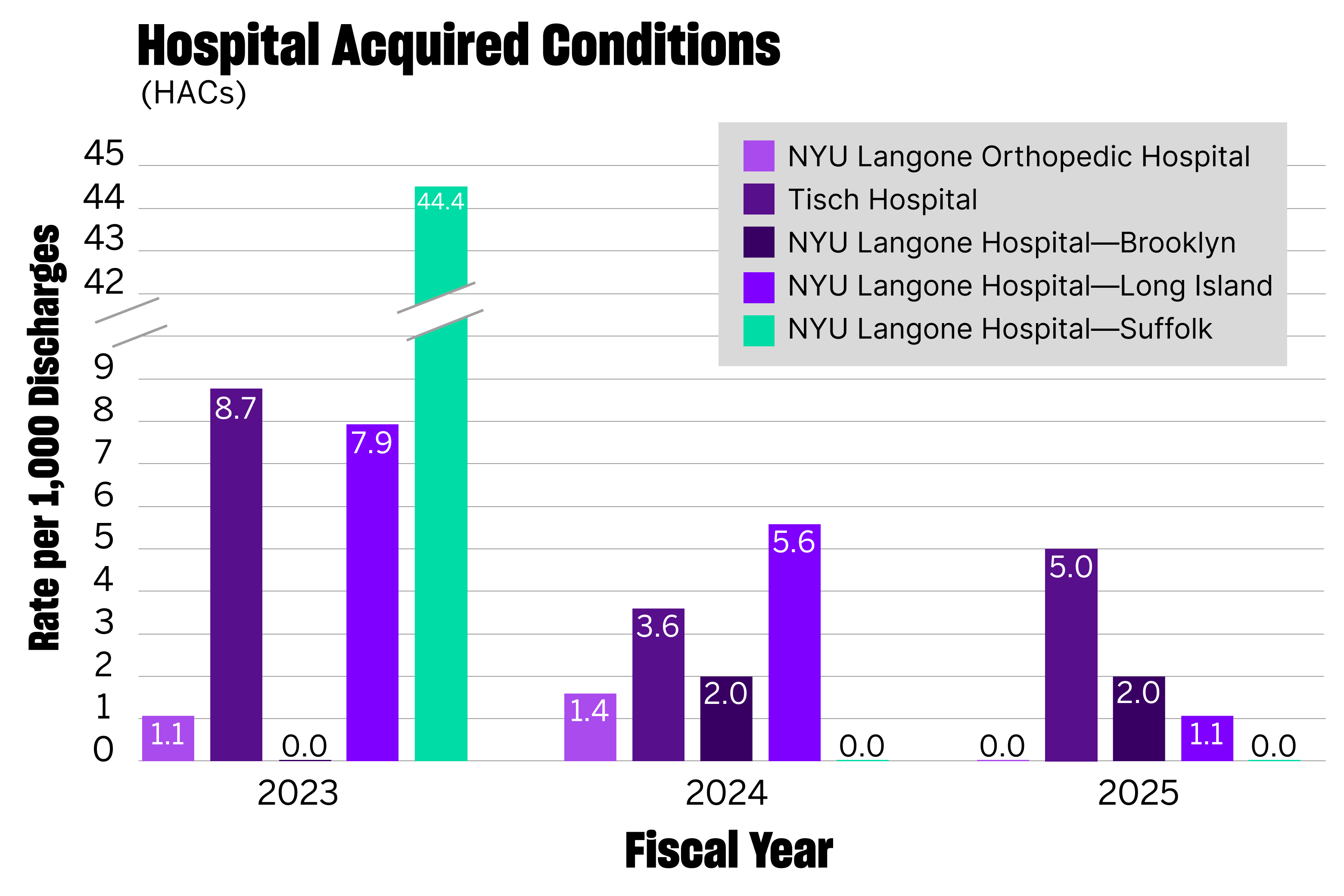
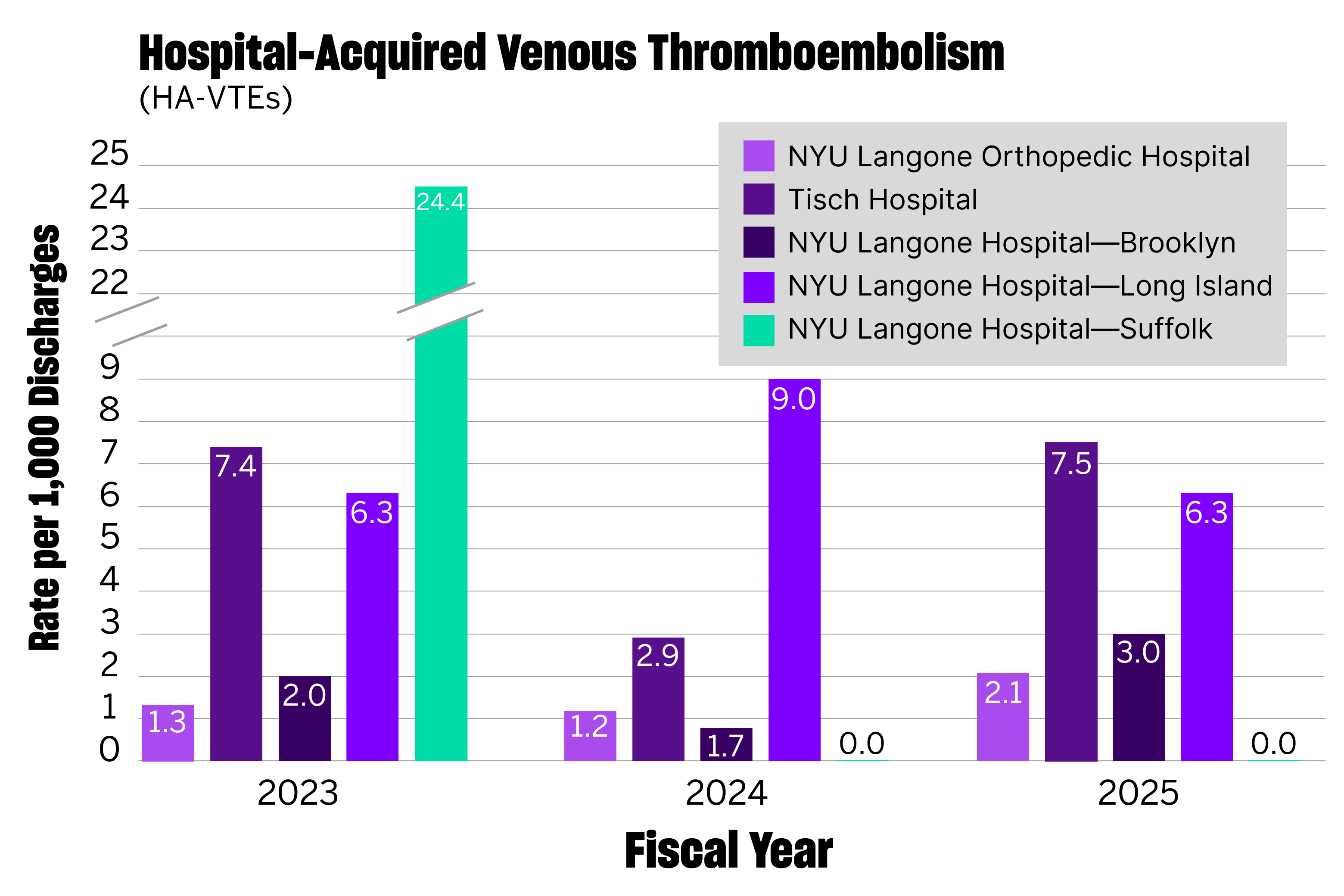
In 2023, the rate of hospital acquired conditions per 1,000 discharges was 44.4 at Suffolk compared to 1.1 at NYU Langone Orthopedic Hospital; hospital-acquired venous thromboembolism (VTE) cases 24.4 and 1.3, respectively.
For orthopedic procedures, on-time starts occurred 19 percent of the time, the mortality rate for patients with hip fracture was 2.5 percent, and only 20 percent of discharges occurred before noon.
Physician Focus: What changes were made to improve the quality of care?
Dr. Savino: One of the first things we established was chief rounds. Leaders went room to room, seeking to understand what was driving the high complication rates.
We discovered that due to issues with the EMR software and phase of care work flows, order sets for antibiotics, VTE prophylaxis, and sequential compression devices were disappearing. We built a technological solution to solve this problem, ensuring that the front-line clinical staff were properly trained on the software. Soon after, the complication rates began to drop.
We also restructured the staffing models to align with our other sites, allowing nurses to spend more time on direct patient care. Other changes included equipment upgrades and the creation of a zero-harm committee.
Dr. Capozzi: It was clear from the beginning that prior leadership was not using a metrics-driven system to track performance and outcomes.
As hospital systems grow in size, their quality often suffers. To achieve a successful system integration, you have to be deliberate and strategic, taking differences across practice settings into account. Where we’ve chosen to merge, our goal is to provide high-quality care regardless of location.
Dr. Lajam: Everyone loves a great comeback story. Once we put NYU Langone’s protocols and performance dashboards in place, there was a rapid improvement in all metrics hospital-wide. The benefit of dashboarding lies in the ability to visualize data and monitor performance in real-time.
“Once we put NYU Langone’s protocols and performance dashboards in place, there was a rapid improvement in all metrics hospital-wide.”
Claudette M. Lajam, MD
Since our dashboard technology and protocols have already proven effective in Manhattan and Long Island, we simply implemented them at Suffolk, ensuring the teams were properly trained. They caught on quickly, and the evidence is reflected in the numbers. It was a textbook example of the old saying: “If you give a man a fish, you feed him for a day; if you teach a man to fish, you feed him for a lifetime.”
Physician Focus: Can you share some of the recent metrics?
Dr. Savino: The transformation has been extraordinary. In 2024, the rate of hospital acquired conditions per 1,000 discharges was 0.0 at Suffolk compared to 1.4 at NYU Langone Orthopedic Hospital; hospital-acquired VTE cases were 0.0 and 1.2, respectively.
For orthopedic procedures, on-time starts now occur 90 percent of the time, the mortality rate for patients with hip fracture dropped to zero, and 40 percent of discharges occur before noon.
To achieve these numbers, we didn’t have to reinvent the wheel. Many of these treatment algorithms and protocols were already in place at other NYU Langone sites. The administration has been quite nimble, which has allowed us to establish these systems and oversee their operation at Suffolk.
Physician Focus: What advice would you give to other healthcare leaders looking to improve their metrics?
Dr. Savino: Effective leadership starts from the top down. As chief of orthopedic surgery, I’m reviewing our numbers constantly—looking at turnovers, on-time starts, complication rates, and ensuring that we have adequate patient volumes. If you don’t understand your numbers, improving your metrics will be very difficult.
Dr. Lajam: To effectively improve quality metrics, staff need to have a driving force. When we help our teams understand the reasons behind our actions, educate them on the significance of their performance, and ensure everyone is aligned, we can truly create a lasting impact.
Physician Focus: What is your long-term vision for orthopedics at NYU Langone Hospital—Suffolk?
Dr. Savino: I want to make Suffolk the best community hospital in the country. We’re in the process of building an ambulatory surgery center, which will enhance the safety and efficiency of orthopedic procedures, ultimately providing a better experience for patients.
Additionally, I’m exploring new ways to integrate the latest advancements in robotic technology and artificial intelligence, including planning educational field trips to learn about best practices and efficiency improvements. Building a culture of lifelong learning is key to actualizing our vision.








