Conventional surgical approaches to repair a hole in the eardrum, or tympanic membrane perforation (TMP), involve using graft material to repair the opening, requiring general anesthesia and accompanied by significant costs that may be shared by patients. This creates potential barriers to treatment for certain groups including older patients, those with cardiopulmonary issues, and patients with a perforation in their only hearing ear.
In a randomized, double-blind, placebo-controlled phase 2 trial, researchers at NYU Langone Health are evaluating the efficacy of a minimally invasive, in-office repair that uses fibroblast growth factor 2 (FGF-2) to regenerate the eardrum in chronic, nonhealing TMPs. As part of the study, patients in the control group receive the same in-office approach, with FGF-2 replaced with sterile water.
“For patients living with TMP who have been avoiding eardrum repair due to a desire to avoid surgery, age, comorbidities, or existing hearing-related concerns, this less invasive approach may offer a viable alternative.”
David R. Friedmann, MD
“A randomized controlled trial like this is the gold standard, but it’s rare in surgery because of the complexity of the trial design and the ability to execute it in an unbiased way,” says neurotologist David R. Friedmann, MD, principal investigator of the study. “Our goal is to produce gold-standard evidence regarding nonsurgical options to treat nonhealing tympanic membrane perforations.”
“If the FGF-2 is successful, it will present a significant change in available treatments as well as the groups of patients we can help,” adds Dr. Friedmann.
Tissue Regeneration Versus Traditional Tympanoplasty
In conventional TMP repair, surgeons use cartilage or other tissue to repair the hole in the operating room. “Certainly with larger perforations of the eardrum, many believe this is the only option for successful closure,” Dr. Friedmann notes. “But the eardrum never looks quite the same and may not vibrate as well as a native eardrum.”
In contrast, the approach under study is performed in an office setting. The growth factor under investigation is soaked into a gelatin sponge and secured in place with several drops of fibrin glue.
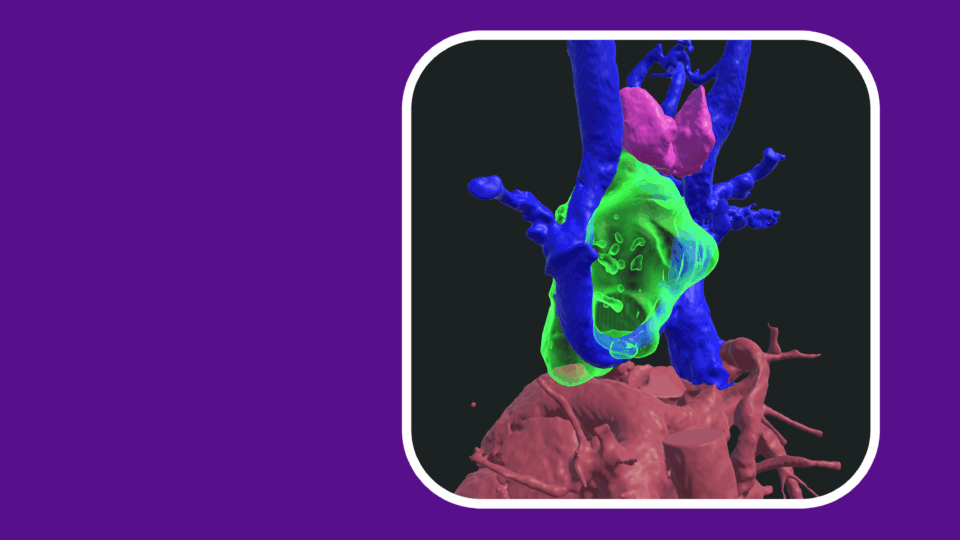
Previous animal studies have demonstrated FGF’s ability to stimulate the division and differentiation of fibroblasts and promote angiogenesis, improve blood flow, and thereby improve closure rates by regenerating the fibrous layer of the eardrum. Images after successful closure often are indistinguishable in appearance and function from a normal eardrum, says Dr. Friedmann.
Study Protocol
In the ongoing trial, participants are randomized to receive FGF-2 or placebo treatment (the same in-office procedure without FGF-2). Subjects randomized to the placebo arm that do not show complete closure after this initial treatment may cross over to receive the active treatment.
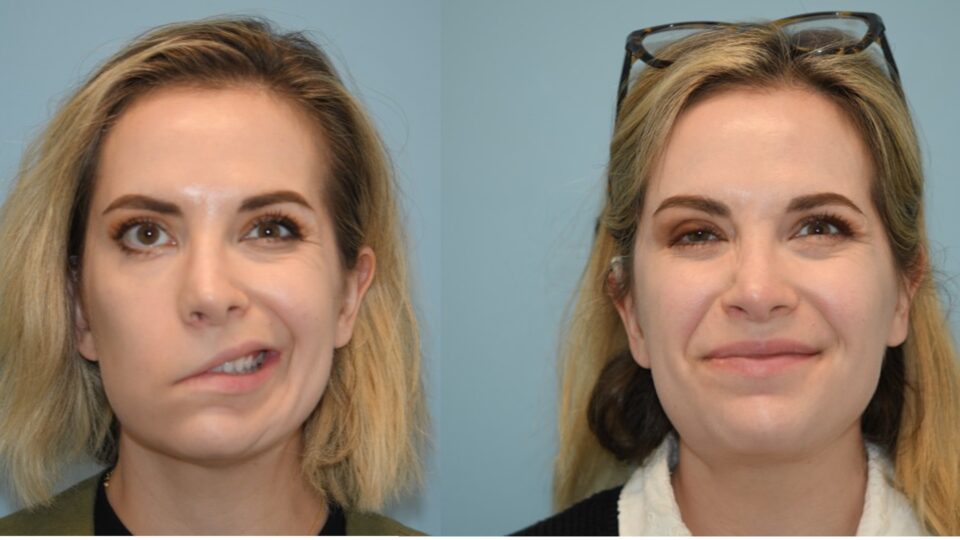
The primary outcome is complete eardrum closure as assessed by pre- and post-treatment photography. Secondary outcomes include time to closure, changes in pure-tone and speech discrimination scores, mobility of tympanic membrane as measured by tympanometry, and salvage rate of FGF-2 in patients who fail placebo treatment.
A New Paradigm for Tympanic Membrane Perforation Treatment
The in-office approach under study is less invasive than conventional surgical treatment.
“Patients can avoid completing preoperative medical testing and labs, and barring unforeseen complications, walk out of the office minutes later, avoiding the need to take time off from work or recover from anesthesia. Additionally, it may be less expensive than conventional surgery,” says Dr. Friedmann.
The trial is open for recruitment through 2023. Both providers and patients are welcome to inquire.
“For patients living with TMP who have been avoiding eardrum repair due to a desire to avoid surgery, age, comorbidities, or existing hearing-related concerns, this less invasive approach may offer a viable alternative,” adds Dr. Friedmann.