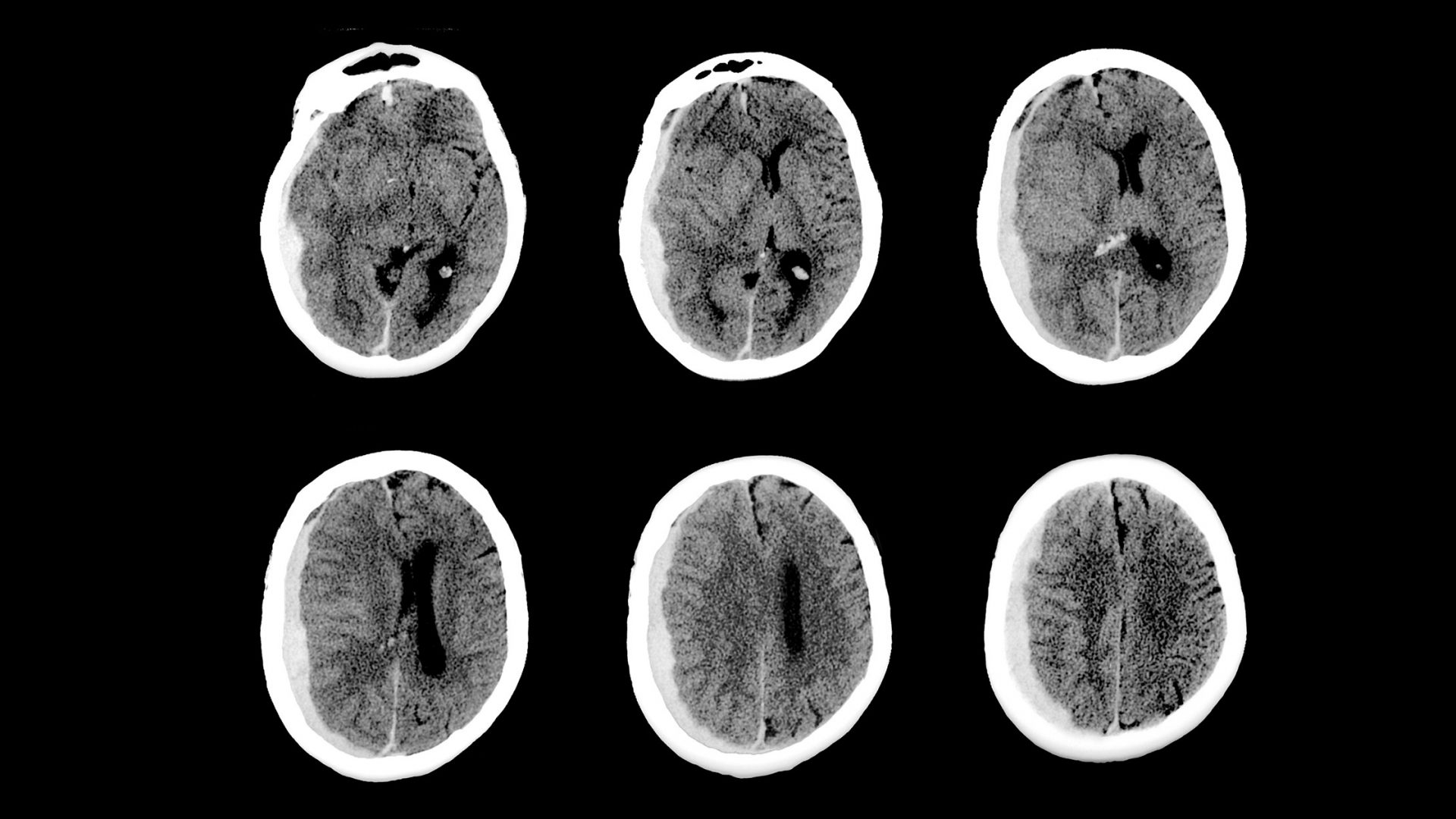
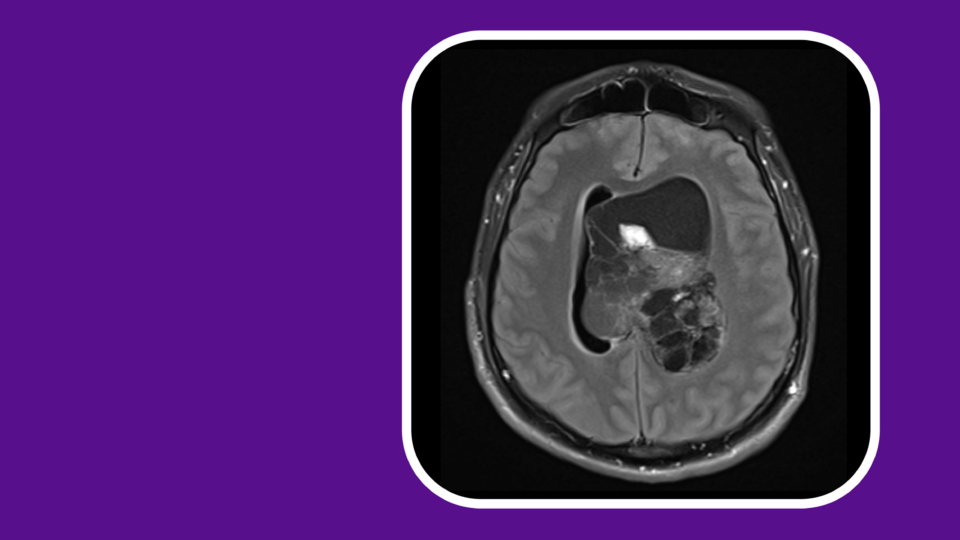
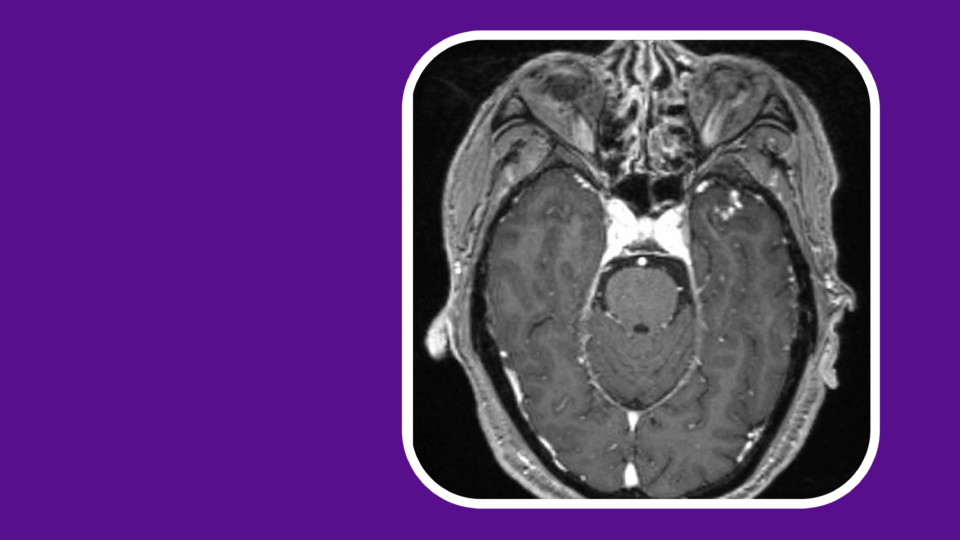
While endovascular embolization using nonadhesive agents is an established method to treat many neurologic disorders, middle meningeal artery (MMA) embolization is a relatively new concept for treating chronic subdural hematomas (SDHs).
In an ongoing clinical trial, NYU Langone Health neurosurgical researchers Eytan Raz, MD, PhD, and Erez Nossek, MD, are examining the safety and efficacy of MMA embolization using SQUID, a potentially best-in-class, low-viscosity liquid particle embolic agent for the management of chronic SDH.
“We have seen some remarkable early results with this procedure in clinical practice.”
Erez Nossek, MD
“We have seen some remarkable early results with this procedure in clinical practice,” Dr. Nossek says. “MMA embolization is a very promising strategy that could potentially revolutionize our ability to care for patients with chronic SDH.”
Collaboration between NYU Langone’s Departments of Neurosurgery and Radiology is making it possible to study the transformative therapy. “In our field, multidisciplinary collaboration is essential,” Dr. Nossek says. “We cannot function without each other.”
Evaluating Treatment Outcomes
Based on promising early results, the researchers are optimistic about the potential for MMA embolization to advance the standard of care and improve the quality of life of patients with this debilitating condition. If the trial results are favorable, it could prompt the FDA to approve the embolic system for this indication.
Unlike patients who receive traditional burr hole drainage, those treated with SQUID could have a reduced likelihood of recurrence and complications. MMA embolization also offers immediate benefits, including a procedural duration of under an hour from start to finish.
“SQUID may assist in resolving some of the current drawbacks of other embolic agents, such as low penetration and visibility.”
Eytan Raz, MD, PhD
“SQUID is a promising nonadhesive, liquid embolic agent that may assist in resolving some of the current drawbacks of other embolic agents, such as low penetration and poor visibility—especially during longer procedures,” Dr. Raz says.
In the trial, patients will receive either MMA embolization with SQUID or standard management without embolization. The primary outcome is treatment failure, defined as residual or re-accumulation of the SDH, re-operation or surgical rescue, or any new, major disabling stroke after enrollment, as well as myocardial infarction or death from any neurologic cause, within six months of the intervention.
“We expect this trial to also provide tremendous insight into the natural history of the disease, which has not been well characterized,” Dr. Nossek adds.
Ensuring Long-Term Safety
The team anticipates the study will yield new insights into the long-term safety of MMA embolization for chronic SDH, explains Dr. Raz, noting that while most prior studies have followed patients for a few weeks post-embolization, the current trial is following patients for six months.
Albeit rare, potential risks of MMA embolization include access artery occlusion and spontaneous dural arteriovenous fistulas. In the study, the team aims to better characterize the risk of these complications as current data are limited.
Ideal Candidates
According to Dr. Raz, embolization of the MMA with SQUID may be particularly useful for patients with comorbidities that require permanent anticoagulation or antiplatelet therapy, especially given that embolization is typically less invasive than open surgery.
“Many patients presenting with chronic SDH are on anticoagulation therapy,” Dr. Raz says. “While surgical evacuation of a chronic SDH requires interruption of anticoagulation therapy, embolization of the MMA using SQUID can be carried out without stopping anticoagulation therapy—this may be a potential safety feature.”
The researchers eagerly await the forthcoming results, which they expect by mid to late 2024.