Acclaimed hematologist–oncologist Anne S. Renteria, MD, has joined NYU Langone Health as site director of the transplantation and cellular therapy program at Perlmutter Cancer Center at NYU Langone Hospital—Long Island. Dr. Renteria will leverage her extensive academic and industry experience to expand stem cell transplant and cellular immunotherapy services.
Previously, Dr. Renteria served as medical director of the stem cell transplant and cellular immunology program at MedStar Georgetown University Hospital, medical director of acute leukemia and stem cell transplant and cellular therapy programs at Rochester Regional Health, and senior medical director of Clinical Development at Forma Therapeutics, a Novo Nordisk company, leading the early clinical development of small molecules for the management of cancer.
Here, she highlights the importance of local access to the latest advancements in bone marrow transplantation and CAR T-cell therapies, shares how her research on treatment underuse and interruptions shapes her priorities, and spotlights a key challenge facing the field of hematology–oncology.
Physician Focus: What inspired you to accept a position at NYU Langone Hospital—Long Island?
Dr. Renteria: I was drawn to the opportunity because Perlmutter Cancer Center at NYU Langone Hospital—Long Island is part of a hospital system that is recognized as being one of the best transplant centers in the world. I was also inspired by NYU Langone’s commitment to increasing patients’ access to care by expanding the size of its workforce.
“It’s important that patients who live on Long Island—or in any area—have access to state-of-the-art care without having to leave their community.”
Anne S. Renteria, MD
With over 7.5 million people living there, Long Island is a busy place with a sizable patient population. Treatment for blood conditions can be an extensive, multistep process. It’s important that patients who live on Long Island—or in any area—have access to state-of-the-art care in leukemia, myeloma, lymphoma, and transplants, including clinical trials when necessary, without having to leave their community.
Physician Focus: Your research addresses barriers to care. Can you share more about this work and your research priorities at NYU Langone?
Dr. Renteria: It’s essential that diverse patient populations benefit from advancements in bone marrow transplantation and CAR T-cell therapies. I was born in New York City, but I have lived in many different countries and speak English, Spanish, Portuguese, and French. I am very sensitive to the nuances of cultural differences and I want to help patients from different backgrounds access the care they need.
“Age, race, ethnicity, and primary insurance contribute to the underuse and unplanned interruptions of multiple myeloma treatment. Those were the findings from our 2021 study.”
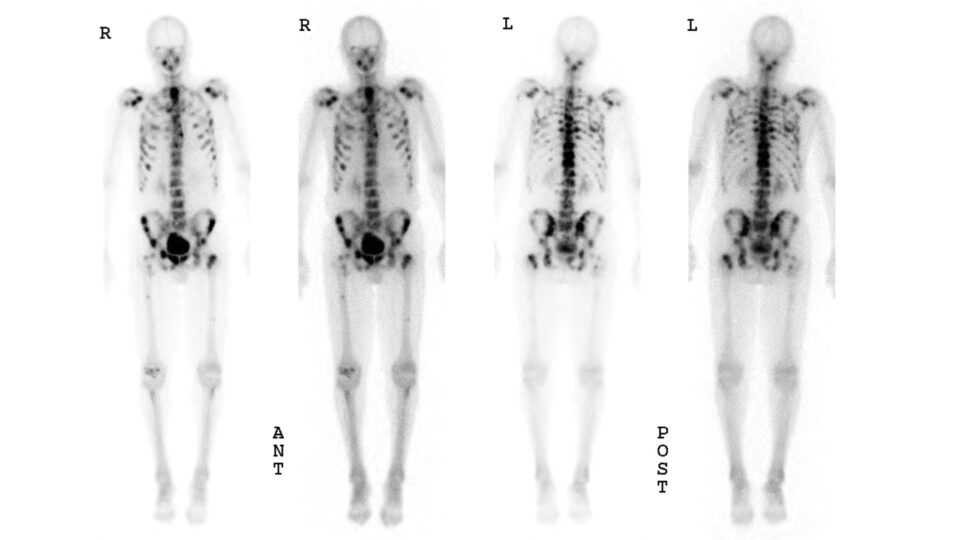
Multiple myeloma, for example, is a complex and costly disease to manage. The expansion of available therapeutic options has inspired optimism regarding disease-related survival. However, age, race, ethnicity, and primary insurance contribute to the underuse and unplanned interruptions of multiple myeloma treatment. Those were the findings from our 2021 study published in Cancer Epidemiology, conducted with Nina Bickell, MD, MPH, and colleagues at Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai.
In my clinical research at NYU Langone, I will collaborate with researchers to investigate how to increase access to care for minorities and how genetic and human leukocyte antigen (HLA) profile differences among ethnic groups affect transplant risks.
Building on my expertise in industry, I am also working with NYU Langone scientists to tailor new treatment modalities in clinical development to specific patient populations, including minorities. There is also a need for older patients to have access to the best possible treatments with less toxicity.
Physician Focus: What are your top priorities as director of the transplantation and cellular therapy program on Long Island?
Dr. Renteria: As site director, my top priority is to work with my team to increase the armamentarium of specialized treatments patients have access to, including autologous and allogeneic transplant and CAR T-cell therapy.
I will also focus on how we as a team, including social workers and nurse navigators, can help patients seamlessly navigate the treatment process, from the moment of their diagnosis through their transition to CAR T-cell transplant.
I also want to create a survivorship program to help patients thrive during blood cancer diagnosis and treatment and achieve the best quality of life possible. Patients are always at the center of my priorities.
Physician Focus: How will blood and marrow transplant services on Long Island fit in with the broader healthcare structure?
Dr. Renteria: We are seeking to expand the blood and marrow transplant program across the NYU Langone system and want to coordinate efforts. Therefore, although I will be based on Long Island, I will be collaborating with colleagues at our other sites, including Jeffrey G. Schneider, MD, chief of the Division of Hematology and Oncology at NYU Langone Hospital—Long Island, Oscar B. Lahoud, MD, chief of hematology at NYU Langone Hospital—Brooklyn, and Mohammad Maher Abdul Hay, MD, director of the Clinical Leukemia Program at Perlmutter Cancer Center.
I will also be working closely with specialties crucial for any transplant service, including the emergency department, critical care, infectious disease, and classic hematology. We need to be mindful of those services every day to provide the best quality of care for our patients.
Physician Focus: What do you consider to be the biggest challenges ahead in the field of bone marrow transplant? How will the Perlmutter Cancer Center and your work aim to address them?
Dr. Renteria: The shortage of physicians and staff is one of the biggest challenges in cancer care in general, and physicians specializing in blood cancer therapy are sorely needed.
“The shortage of physicians and staff is one of the biggest challenges in cancer care.”
Transplant, which is one word that represents different procedures under the same umbrella, is a highly intense field and specialty. It takes a village, including highly trained physicians who specialize in blood and marrow transplantation, advanced practice providers, transplant coordinators, social workers, nutritionists, physical therapists, symptoms management specialists, and others to provide each patient with the best care possible.
To increase the hematology–oncology workforce, we need to understand what hematologist–oncologists, advanced practice providers, nurses, and other team members need to enjoy continuing to work in this field, while tailoring this workforce to meet the patient’s needs.
With a dedicated hematology–oncology service in the community, my hope is that we will not only support patients locally, but also drive new talent to the field and increase retention.