Over the last several years, NYU Langone Health has built a rapidly growing program to expand access to lung cancer screening, regardless of a patient’s ability to pay. This effort is not only improving early detection, but also increasing the frequency at which physicians are faced with complex decisions about nonspecific lung nodules.
“About 30 percent of people getting lung cancer screening will have nonspecific nodules, and we don’t know what they mean,” says Abraham Chachoua, MD, director of the Lung Cancer Center at Perlmutter Cancer Center. “The question is, which one of those nodules is going to change? And can we predict that earlier?”
To pave the way for clear, informed treatment recommendations for nonspecific lung nodules, NYU Langone investigators have launched several research projects and clinical initiatives, all with the central focus of better understanding which nodules are and are not likely to be cancerous.
A Focus on Risk Factors in Nonsmokers
To elucidate risk factors and biomarkers, the investigators have turned their attention to the surprisingly high proportion of lung cancers in nonsmokers.
“Between 15 to 20 percent of lung cancers are found in nonsmokers,” says Dr. Chachoua. “This is a different disease in terms of molecular features. Even the demographics tend to be younger.”
An initial focus of this work is on Asian women. Over 40 percent of Asian women diagnosed with lung cancer are nonsmokers—roughly double the rate of the general population—and the cause is unclear.
In an ongoing three-year study led by Elaine Shum, MD, an oncologist and assistant professor of medicine, nonsmoking Asian American women in the New York City area will receive an annual low-dose CT chest scan, donate blood samples, and provide information on family history and environmental and World Trade Center dust exposures.
The goal is two-pronged: to determine lung cancer incidence in Asian American women and build a database and biorepository that can be used to identify factors that contribute to the development of cancerous nodules.
“As we continue to screen, we are also gathering important information to better understand the pathogenesis of lung cancer.”
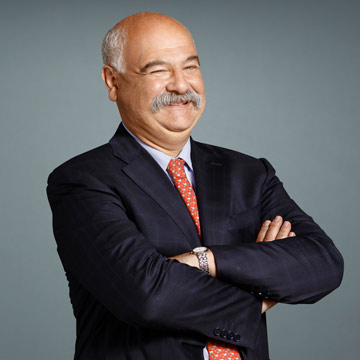
Abraham Chachoua, MD
Currently, there are over 80 participants enrolled, of which 73 have completed initial CT scans. “Two cancers have been found in this group, which is an incidence of 2.7 percent. That is similar to the incidence of lung cancer in smokers,” Dr. Chachoua says.
“Our study continues to increase its enrollment, but these early cases are encouraging that our idea to screen another potential high-risk population may be of benefit,” Dr. Shum adds. “As we continue to screen, we are also gathering important information to better understand the pathogenesis of lung cancer, not just in Asian women nonsmokers but in all nonsmokers.”
Detecting Patterns in DNA Fragments
A concurrent biomarker study is assessing whether fragments of tumor DNA in peripheral blood yield patterns indicative of lung cancer. The study is led by Dr. Shum, Kwok-Kin Wong, MD, PhD, director of the Division of Hematology and Medical Oncology, and Jun-Chieh J. Tsay, MD, an assistant professor of medicine, in collaboration with Delfi Diagnostics.
The goal is to assess whether patients who are screened and ultimately found to have cancerous nodules have a different DNA fragmentation pattern than those who are screened and aren’t found to have lung cancer.
“All of the patients enrolled in our study of lung cancer in nonsmoking Asian American females have had this test done,” explains Dr. Chachoua. “It will be interesting to see whether the two patients identified with cancer will have unique signatures by DNA fragmentation. That will be a big innovation for the field.”
Diverse Research Ahead
Additional research projects on the horizon will evaluate whether breath tests or readouts from the lung microbiome can be used to detect cancerous nodules. Dr. Chachoua also notes an interest addressing why a low percentage of patients eligible for screening come in to receive a scan.
“We’ve had 655 referrals since we started the lung cancer screening program. About 40 percent are eligible for screening, and out of the eligible patients only 67 percent got their scan,” Dr. Chachoua says. “We’re going to do a population science study in that area to address the gap.”
Assembling Experts to Review Nonspecific Nodules
Another notable development is the formation of a lung nodule review board, which reviews all nodules with Lung-RADS scores of 3 or 4—those that are of high suspicion to become cancer.
“After forming this dedicated team, we found that about 26 percent of the reports changed, and some of those changes led to earlier identification of cancers,” Dr. Chachoua says.
Dr. Chachoua says a full account of how the review board is helping to elevate the treatment of suspicious nodules will be presented at an upcoming national meeting.