A child with spastic diplegia secondary to cerebral palsy experienced a smooth recovery after surgeons at NYU Langone Health performed a successful selective dorsal rhizotomy (SDR).
The 7-year-old patient was referred to Hassenfeld Children’s Hospital for multidisciplinary evaluation by pediatric neurosurgeon David H. Harter, MD, the attending surgeon on the case, and pediatric physiatrist Patricia T. Tan, MD. “Within days of the surgery, we saw significant improvements in energy levels, motor function, and spasticity,” says Dr. Harter. “His mom is overjoyed, sharing that just six months after surgery he was ambulating independently and riding a specialized bike.”
“It was remarkable to see how quickly he responded to the procedure.”
David H. Harter, MD
Born prematurely at 37 weeks, the patient’s medical history was complicated by vascular ring anomaly, chromosome P deletion, tracheomalacia, gastroesophageal reflux, and constipation. According to his mother, he also experienced perineal numbness and had persistent difficulties with bowel training. The patient had undergone several orthopedic procedures and received oral baclofen with limited success.
Unlike other interventions, SDR addresses the root cause of spasticity rather than solely alleviating symptoms. “It was remarkable to see how quickly he responded to the procedure,” says Dr. Harter.
Expertise in SDR
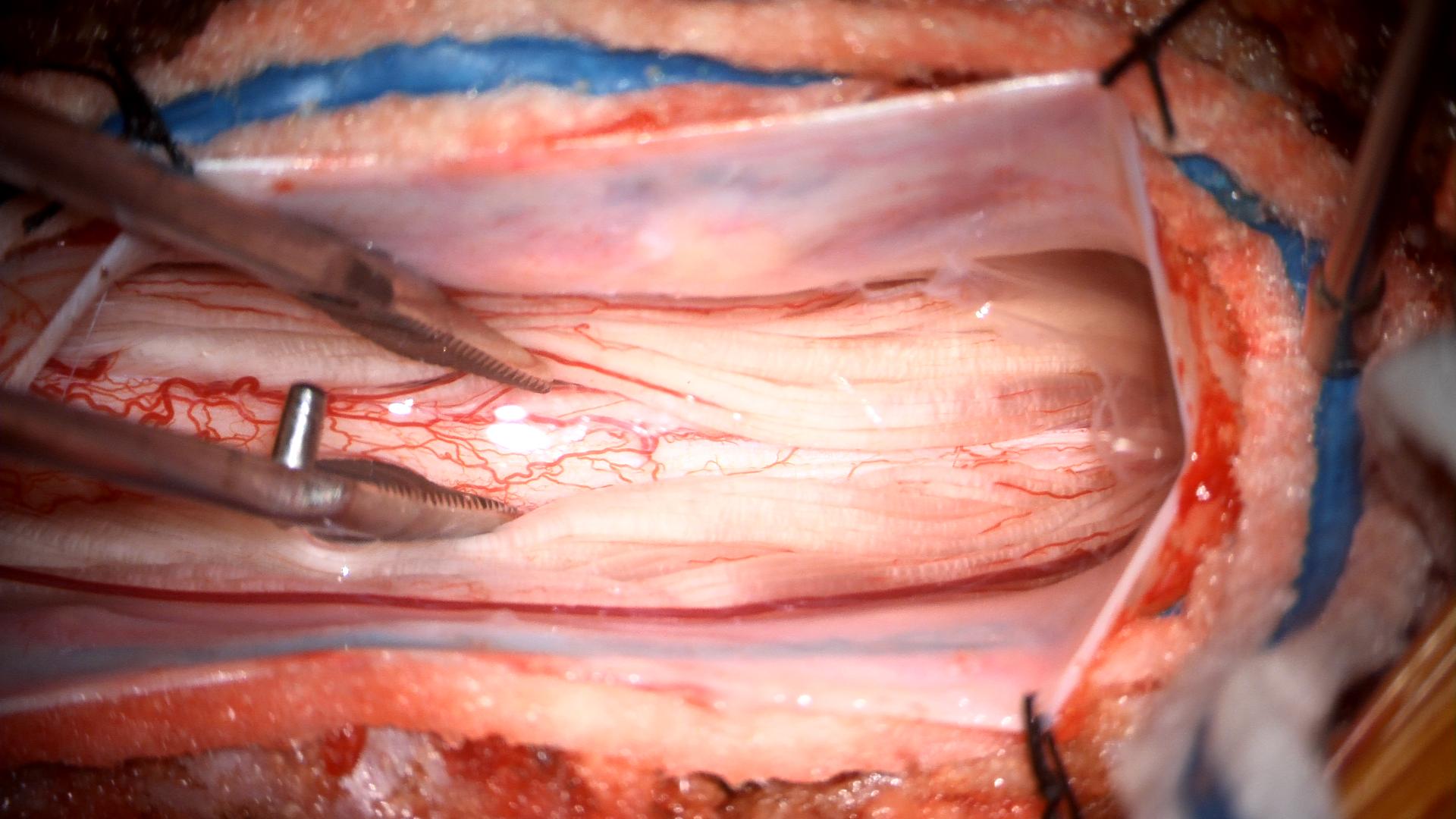
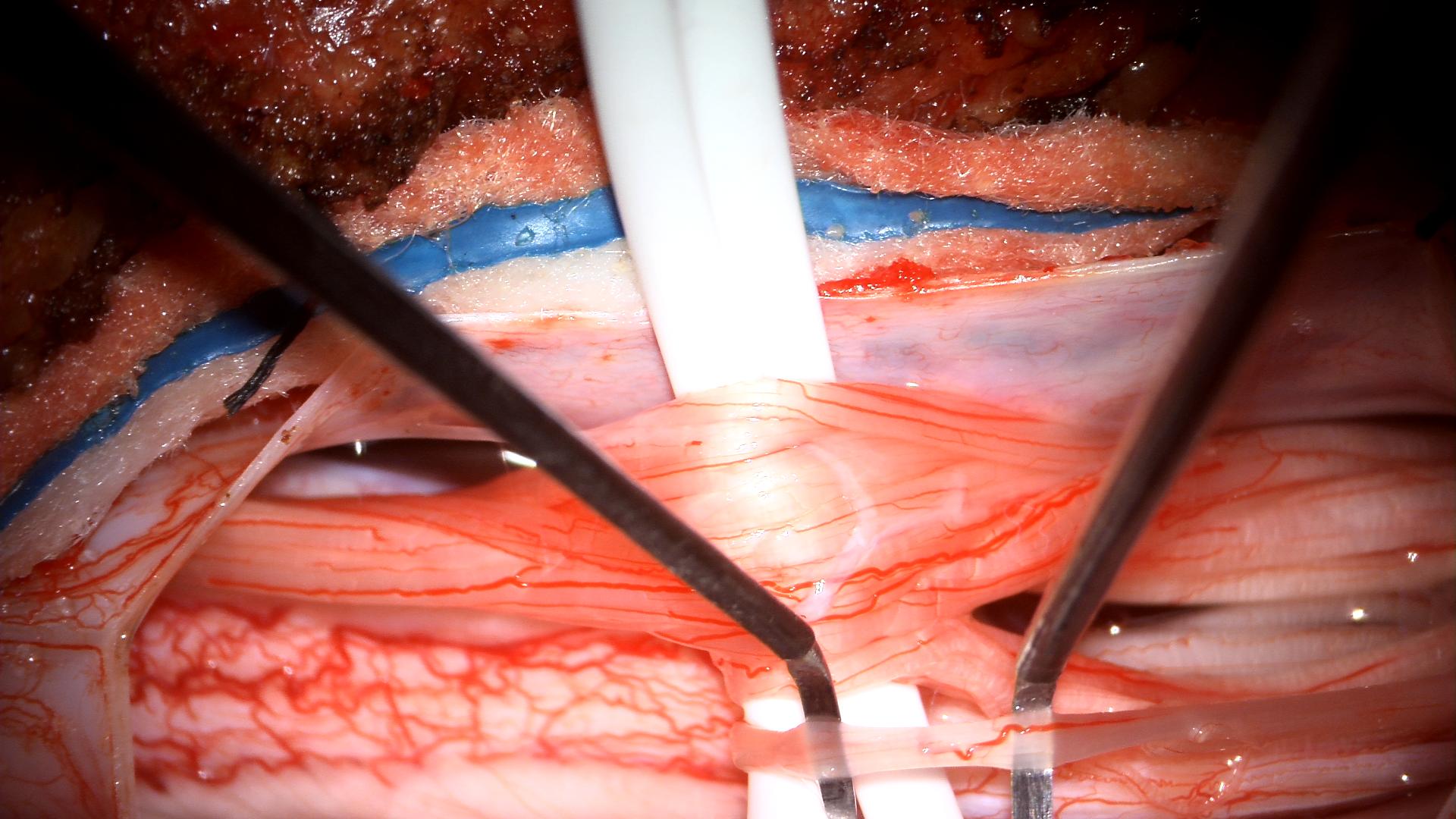
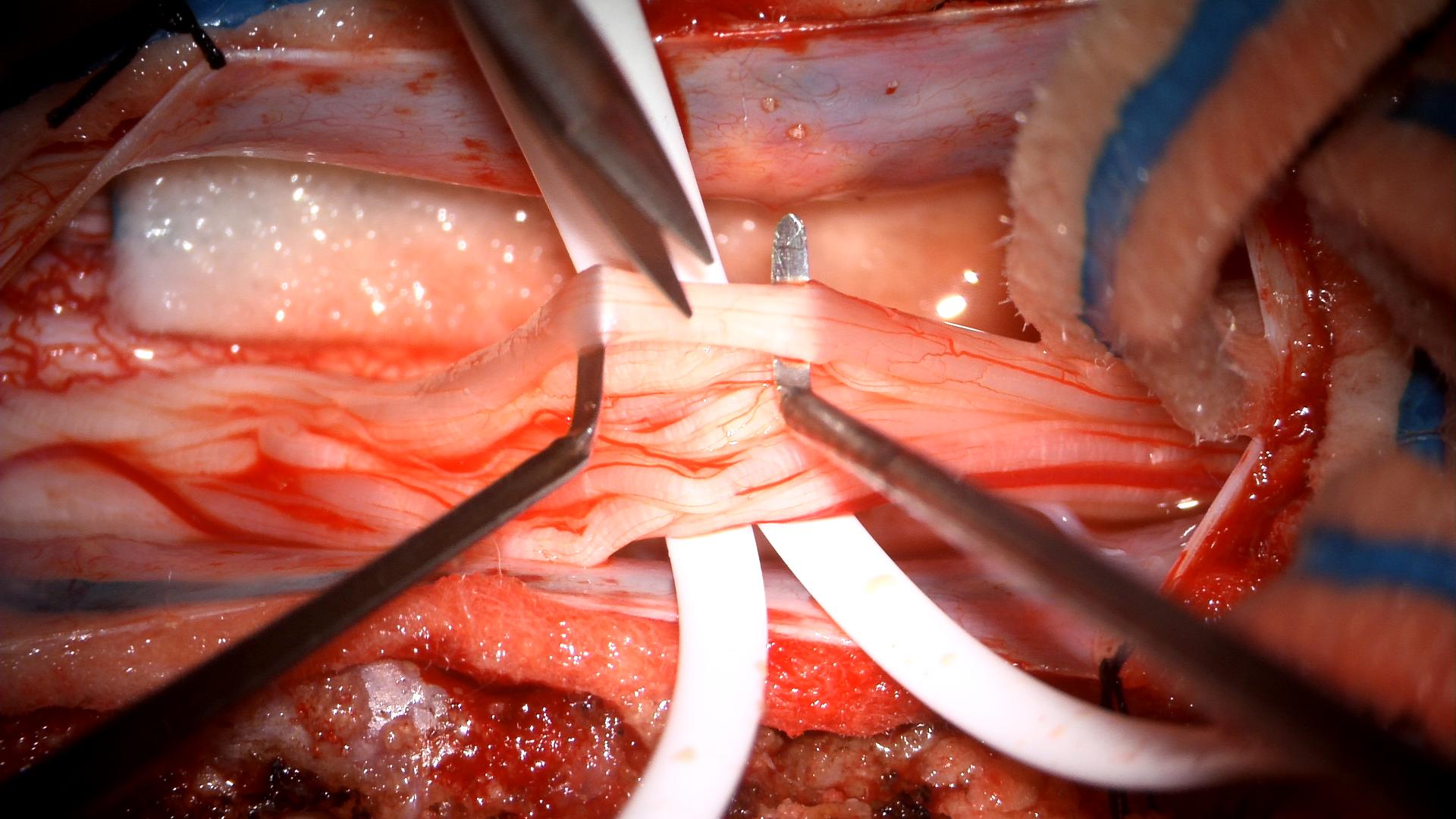
NYU Langone is a high-volume center for SDR, a procedure that permanently reduces lower limb spasticity in children with spastic diplegic cerebral palsy by selectively severing sensory nerve fibers in the spinal cord. This spasticity leads to motor difficulties, evolving as muscle shortening, tendon contractures, and rotational bone and joint deformities. As patients grow, they may develop a crouch gait that can hinder their ability to ambulate.
“Reducing spasticity in children with cerebral palsy can have positive effects on their growth and development,” says Dr. Harter. “SDR is associated with few complications and excellent long-term outcomes.”
Restoring Function and Independence
Dr. Harter and colleagues used magnetic resonance imaging (MRI) of the brain and spine to determine the patient’s eligibility for surgery. The brain MRI showed changes related to bilateral germinal matrix hemorrhage, with no evidence of hydrocephalus, while spine MRI ruled out intraspinal pathology.
“Given his cognitive status, lack of involvement of the upper extremities, and his eagerness to participate in therapy and exercise, we knew he would be an ideal candidate for an elective procedure,” says Dr. Harter.
The surgery was performed without complication, and the patient’s recovery was swift. Two weeks after surgery, he demonstrated significant improvements in motor function and posture, completing intensive inpatient rehabilitation with Rusk Rehabilitation. Upon discharge, the Rusk team coordinated ongoing outpatient rehabilitation with local physical therapists near the patient’s home.
“Going in, we were confident in our team’s planning and expertise,” says Dr. Harter, “which involved the coordination of outpatient rehabilitation services close to home.”