Seamless collaboration between pediatric specialists at Hassenfeld Children’s Hospital at NYU Langone and adult providers at NYU Langone Health enabled an 11-year-old patient’s tracheal tumor, blocking 85 percent of the airway, to successfully be resected in less than 2 hours using robotic surgery.
The outcome demonstrates the pivotal strengths that come with having continuity between children’s and adult services.
“This procedure could not have been done at any other children’s hospital,” says Jason C. Fisher, MD, surgical director of the Pediatric ECMO Program. Dr. Fisher managed heparin-free extracorporeal membrane oxygenation (ECMO) support during the operation, minimizing the risk of surgical bleeding.
“Because we had the expertise to do it robotically, the tumor was removed with only four small incisions, and it took less than an hour and a half.”
Jason C. Fisher, MD
“Because we had the expertise to do it robotically, the tumor was removed with only four small incisions, and it took less than an hour and a half,” says Dr. Fisher.
Making All the Right Moves
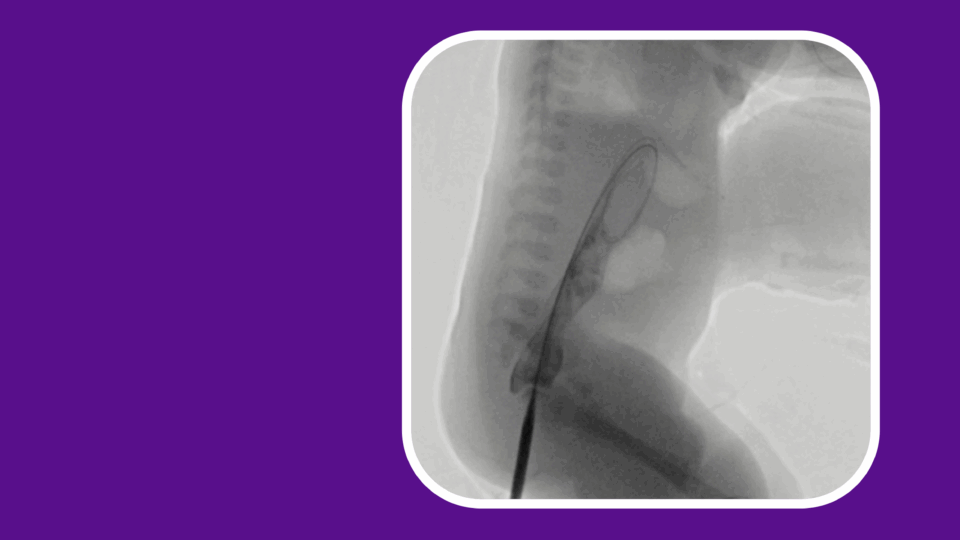
The patient was admitted to the pediatric ICU for difficulty breathing, hypoxia, and other symptoms initially attributed to COVID-19. Although she responded to treatment, a chest CT was performed to understand the cause of a pneumothorax leaking air into the space between the lungs and the chest wall and up into the neck.
That’s when the care team saw that a mass located close to the carina was causing a near-complete obstruction of the trachea.
To collect a biopsy and debulk the tumor, pediatric pulmonologist Eleanor Muise, MD, and Jamie L. Bessich, MD, an interventional pulmonologist with the adult hospital, performed a rigid bronchoscopy.
“That was a very elegant procedure. It enabled us to not only collect a tissue sample to direct definitive treatment but also ablate part of the tumor so that airway obstruction was no longer an imminent concern.”
Eleanor Muise, MD
“That was a very elegant procedure,” says Dr. Muise. “It enabled us to not only collect a tissue sample to direct definitive treatment but also ablate part of the tumor so that airway obstruction was no longer an imminent concern.”
During the procedure, Dr. Fisher was ready with ECMO support in case the airway became occluded. “We didn’t need to put her on, but we had a pump and a team on standby,” he says.
ECMO without Heparin
Biopsy confirmed the tumor to be a soft tissue mass requiring tracheal resection and reconstruction, and world-renowned thoracic surgeon Robert J. Cerfolio, MD, MBA, performed the operation using a minimally invasive robotic approach.
“There are no pediatric surgical specialists who can do what Dr. Cerfolio can do,” says Dr. Fisher. “The type of robotic surgery he does is in a league of its own. And he is right next door.”
To optimize exposure and eliminate the need to ventilate the lungs during surgery, Dr. Fisher put the patient on ECMO. He and his team managed ECMO support without an anticoagulant, having deemed the risk of bleeding during the operation to be higher than the risk of clotting.
“We have a very successful pediatric ECMO program, and we made the calculation that, based on the patient’s size, we could flow through the pump fast enough and that Dr. Cerfolio could operate with such efficiency that we could run ECMO without heparin,” says Dr. Fisher. “We were confident in our team’s approach, and we planned this well.”
An Excellent Prognosis
The patient will only require close follow-up as staging confirmed the cancer had not spread. Dr. Muise also completed a repeat bronchoscopy after the procedure, stating the tracheal anastomosis to be “beautiful and widely patent,” with no visual indication of abnormal mucosa in the area.
“That’s what we customarily do when we see more of an adult type of tumor in a child, ask for advice, and work collaboratively with our adult partners who see these far more often than we do. We’re so fortunate that we have the capabilities of doing that here at the medical center.”
Elizabeth A. Raetz, MD
The tumor was ultimately determined to be a low-grade mucoepidermoid carcinoma, a type of salivary gland tumor more commonly seen in adults. Results from the NYU Langone FUSION-SEQer test revealed the specific gene fusion, CRTC3-MAML2, that helped confirm the diagnosis. Colleagues in pediatric hematology–oncology Nicole Mallory, MD, and Elizabeth A. Raetz, MD, consulted on the case, which was also presented to adult specialists at a tumor board.
“That’s what we customarily do when we see more of an adult type of tumor in a child, ask for advice and work collaboratively with our adult partners who see these far more often than we do,” says Dr. Raetz. “We’re so fortunate that we have the capabilities of doing that here at the medical center.”