Fortuitous CT Reveals Hidden Tracheal Tumor
A pediatric patient with a large tracheal tumor is cancer free after specialists at NYU Langone Health and Perlmutter Cancer Center teamed up to safely diagnose and resect the unusual growth. The patient presented to the pediatric intensive care unit at Hassenfeld Children’s Hospital for respiratory sequelae initially attributed to COVID-19 when the mass was detected by CT.
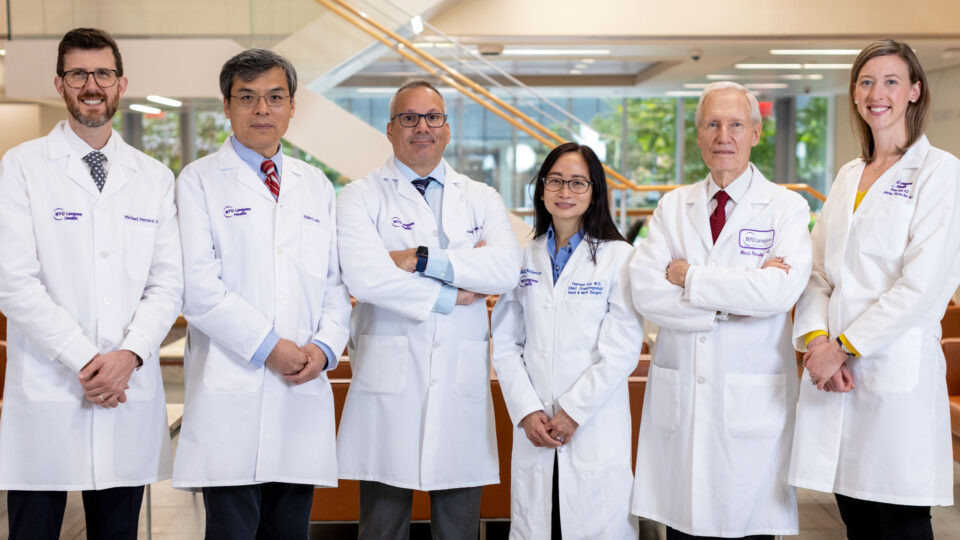
“This team worked together seamlessly, drawing on every person’s expertise and strengths to do the best thing for the patient,” says Jamie L. Bessich, MD, an interventional pulmonologist assisting on the case. “We enjoy seeing each other work at such a high level.”
“This team worked together seamlessly, drawing on every person’s expertise and strengths to do the best thing for the patient.”
Jamie L. Bessich, MD
The mass emanated into the trachea from the posterior wall and blocked roughly 85 percent of the airway. The best treatment was determined to be surgical resection, but a biopsy was performed first to rule out lymphoma or other conditions not requiring major surgery.
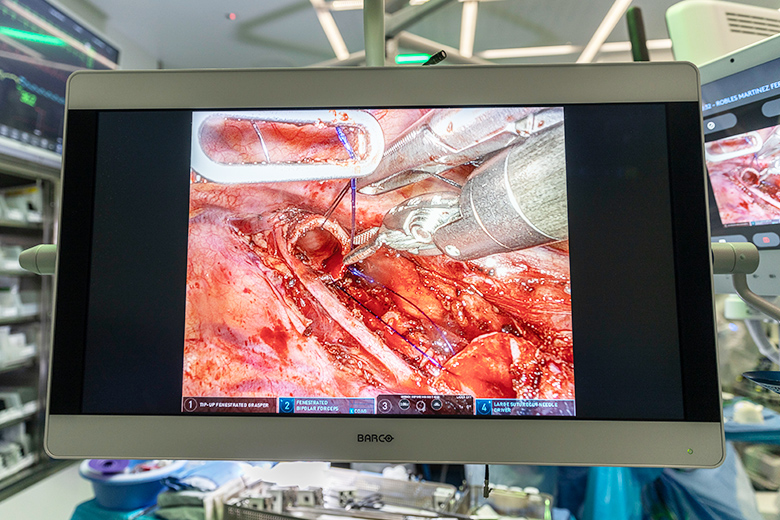
Dr. Bessich and pediatric pulmonologist Eleanor Muise, MD, performed the biopsy using rigid bronchoscopy, chosen over flexible bronchoscopy for the ability to ventilate the airway. During the procedure, ablative therapy was also administered to excise a large portion of the tumor and minimize any risk of obstruction before surgery.
“This was the youngest patient I’d ever seen with a tracheal mass, and it was the second youngest patient I’d ever performed a rigid bronchoscopy on,” says Dr. Bessich.
When the biopsy confirmed that surgery was required, the patient was immediately scheduled, with pediatric surgeon Jason C. Fisher, MD, placing the patient on venovenous extracorporeal membrane oxygenation (VV ECMO) and thoracic surgeon Robert J. Cerfolio, MD, chief of clinical thoracic surgery, performing the minimally invasive operation.
“We are one of only a few centers in the world that can do this without opening the chest and on ECMO.”
Robert J. Cerfolio, MD
“We are one of only a few centers in the world that can do this without opening the chest and on ECMO,” says Dr. Cerfolio.
Pathology and genetic analyses ultimately determined the tumor to be a low-grade mucoepidermoid carcinoma. With no signs of metastasis, it is unlikely that radiation or chemotherapy will be required.