Case Highlights:
- The patient had a long history of multiple spinal fusions involving the entire spine, MS, and osteoporosis; she had limited independent mobility due to back pain and leg weakness.
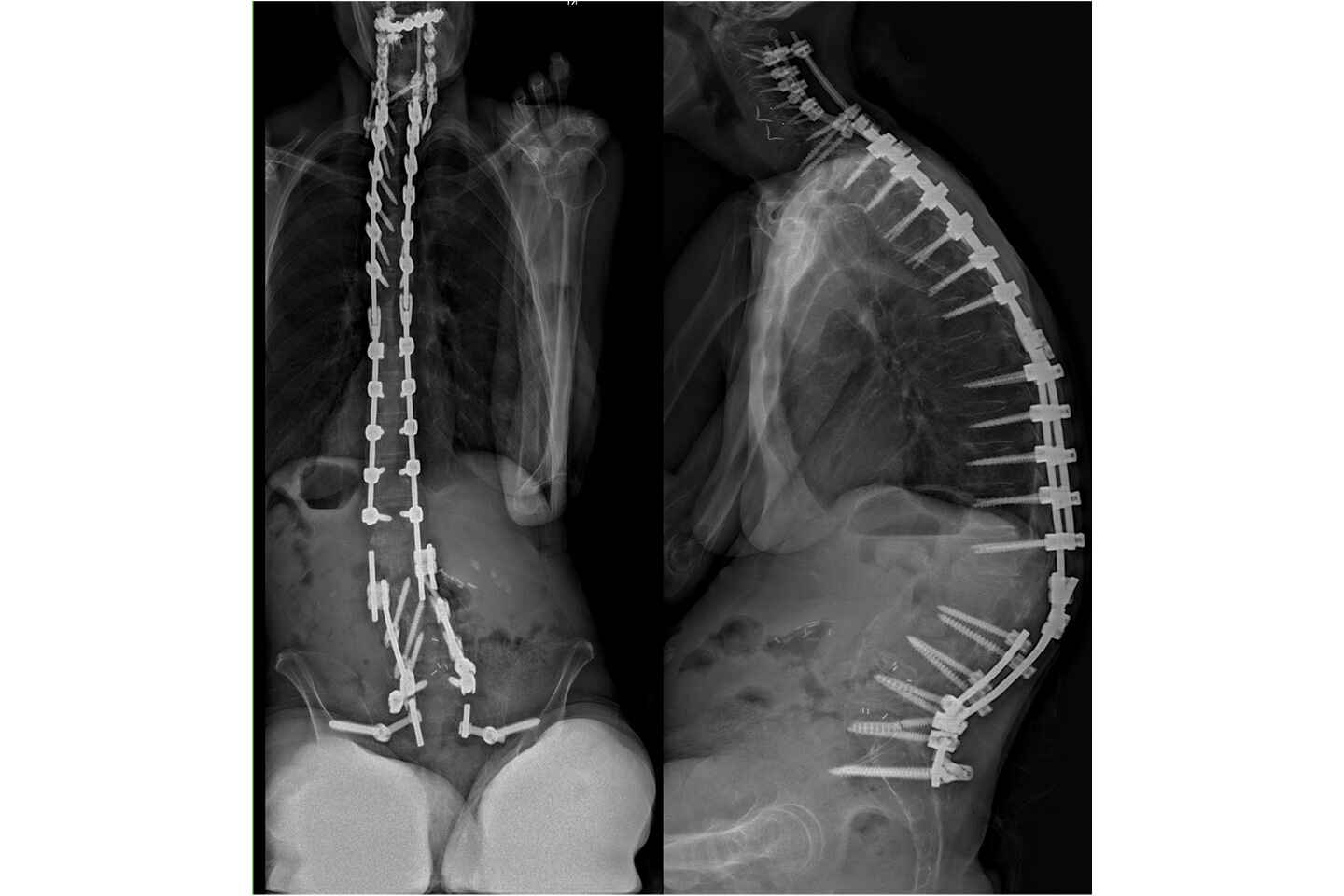
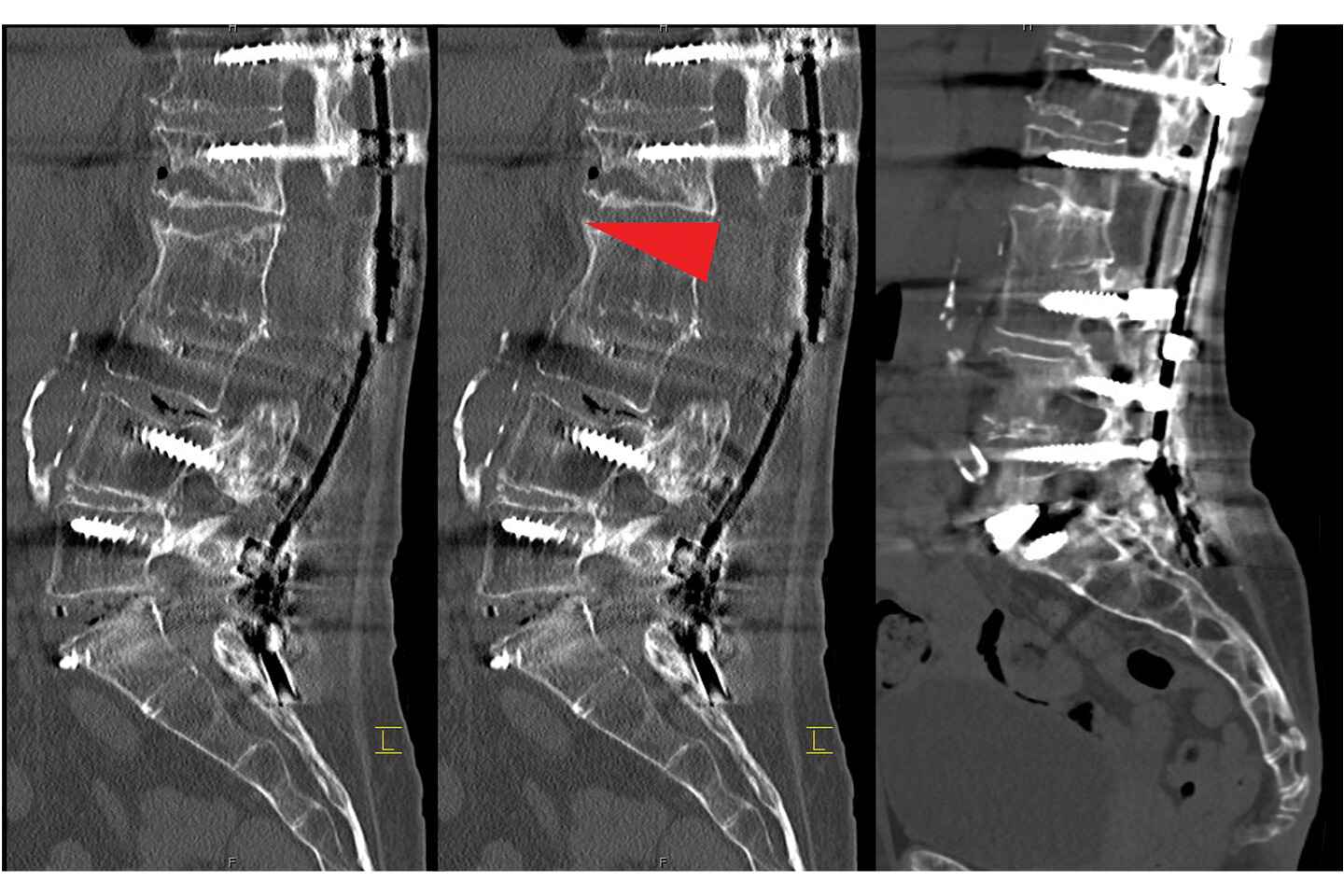
- Imaging revealed a prior instrumented fusion from C2 to the pelvis with multiple rod fractures, pseudoarthrosis, and severe spinal deformity (kyphoscoliosis).
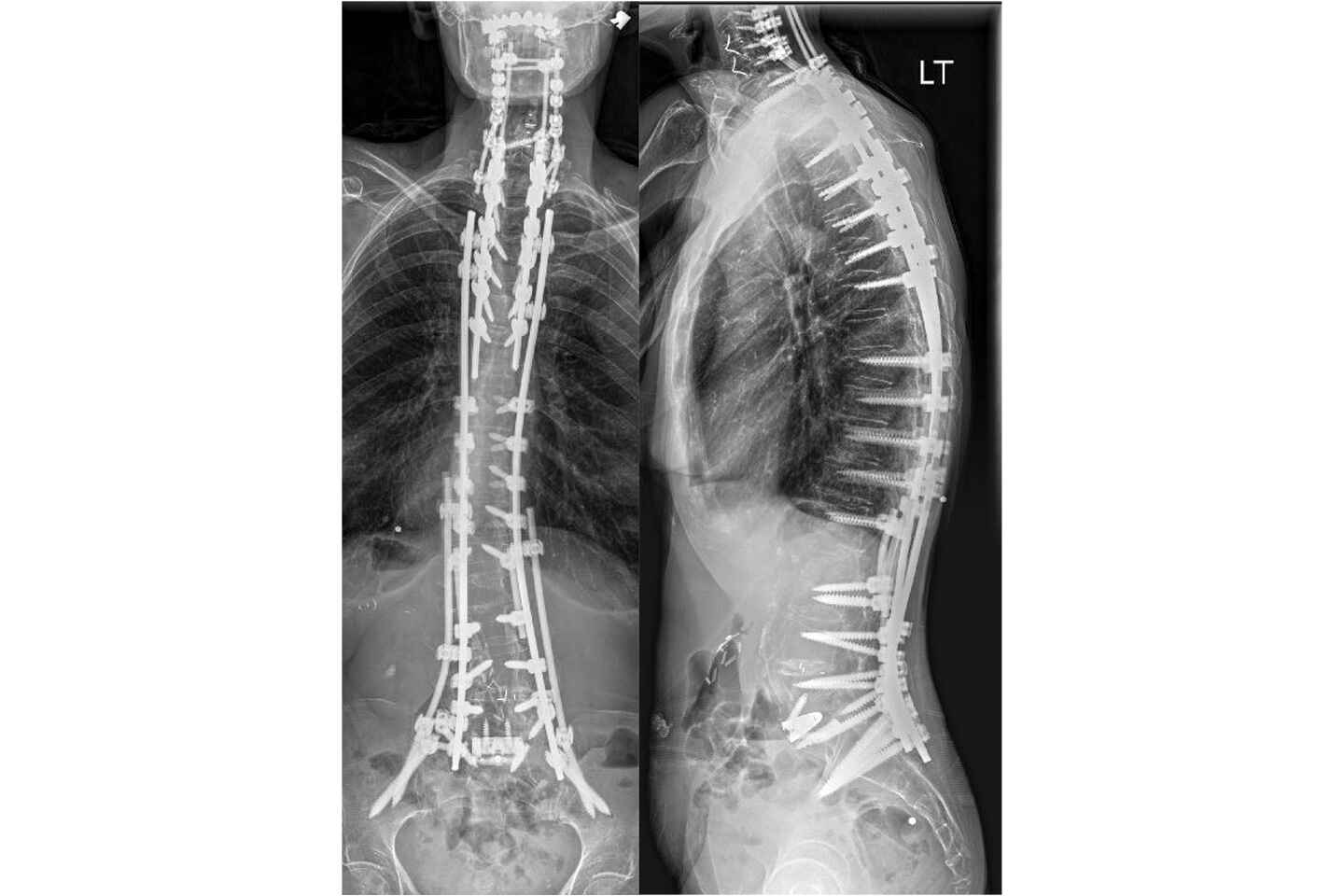
- Neurosurgeons performed an L5-SI anterior lumbar interbody fusion, revision T4 to pelvis posterior spinal fusion, and L2 PSO.
- Three months post-surgery, the patient reported no pain and was able to walk without a walker for the first time in years.
In March 2024, a female in her 60s who had previously undergone multiple spinal fusions presented to NYU Langone Health with unrelenting and progressive back pain, an inability to walk, and a sense of hopelessness. She was essentially homebound from her spinal condition and required a wheelchair, with minimal ability to walk short distances with a walker. The patient had a complicated medical history that included a cerebral aneurysm, multiple sclerosis (MS), and osteoporosis.
X-ray imaging revealed multiple prior fusions connected together from C2 to the pelvis. The rods were clearly fractured in multiple places. The combination of rod fracture and failure, together with pseudoarthrosis, had led to a severe and progressive spinal deformity. Extensive nonoperative treatments had failed to bring relief and multiple surgeons and intuitions had told her there were no other options.
“Everyone had given up on this patient before she saw me. This was really her last resort.”
Darryl Lau, MD
“Everyone had given up on this patient before she saw me,” says neurosurgeon Darryl Lau, MD, director of complex spine and adult spinal deformity at NYU Langone. “This was really her last resort but I remained confident that we could help her and do it safely.”
To relieve the end-stage spine disease, alleviate her chronic pain, and prevent her from becoming permanently wheelchair-bound, Dr. Lau and colleagues performed a two-staged surgery involving a reconstructive spinal fusion and a pedicle subtraction osteotomy (PSO), a surgery not offered by most spine surgeons.
Staged Approach
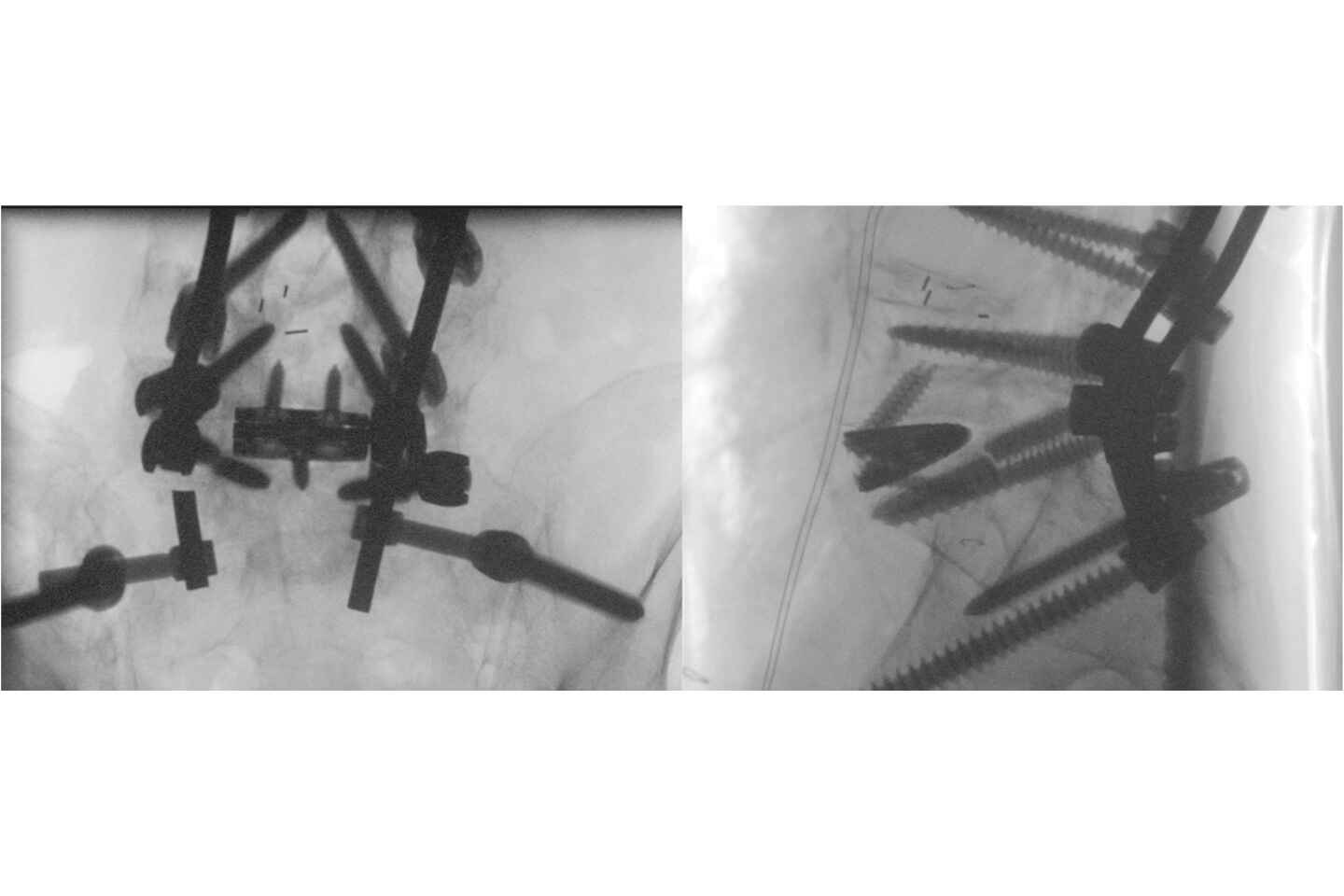
In the initial surgery, performed in July 2024, Dr. Lau and vascular surgeon Leon K. Eisen, MD, performed an L5-SI anterior lumbar interbody fusion (ALIF) to revise the failed fusion and start to correct the severe deformity. A failed interbody cage was removed and replaced with a patient-specific titanium cage and bone graft to encourage bone regeneration.
In a more extensive follow-up surgery two days later, Dr. Lau and colleagues revised her failed fusion construct from T4 to the pelvis and performed an L2 PSO to reshape and reconstruct the spine into a harmonious physiologic alignment.
“These patients undergo very invasive but needed surgery with large incisions,” Dr. Lau says. “Essentially, we mobilize the spine by carefully removing part of the spinal column to correct the deformity and secure it in place with the revised fusion construct.”
The team implanted patient-specific, custom-made cobalt chrome rods—designed with novel AI technology—to stabilize the spine in its newly corrected position. Reconstructive plastic surgeon Michael S. Margiotta, MD, performed the complex spine closure.
Expertise to Support ‘Controlled Trauma’
Through its ability to optimize patients preoperatively, intraoperatively, and postoperatively, Dr. Lau says, NYU Langone is among the few medical centers that can safely perform this series of procedures for such exceedingly complex patients. “The stress it takes for the body to handle this type of controlled trauma is pretty tremendous,” he says.
“Why do we do something like this? We do it because it enables the most disabled pain patients to be free from pain and off medications.”
The success of the case relied on the expertise and close collaboration of NYU Langone’s surgeons, anesthesiologists, ICU providers, and other specialists. The patient’s presurgical optimization entailed extensive anabolic bone therapy in collaboration with rheumatologists. Thorough post-surgical monitoring and treatment in the ICU, in turn, was essential for avoiding complications and resolving conditions such as the expected anemia due to acute blood loss.
The patient’s strong support network was also instrumental to the success of the operation and a major factor in the decision to proceed.
A Life-Changing Resolution
One key to preventing these complex and traumatic surgeries later in life, Dr. Lau says, is performing the right initial surgery with a careful analysis and understanding of the patient’s spinal shape. Without that attention to detail, multiple surgeries can leave the spine completely malaligned, he says, leading to recurrent spinal problems, implant failures, and chronic pain.
At the patient’s three-month follow-up, she reported that her back felt “great,” with essentially no pain. Unexpectedly for both her and her neurologist, she also regained the ability to walk independently despite her MS.
“Why do we do something like this? We do it because it enables the most disabled pain patients to be free from pain and off medications,” Dr. Lau says. “The results can be dramatic and life-changing.”