Referral Notes:
- NYU Langone researchers have conducted the first meta-analysis of adverse psychiatric outcomes in randomized, controlled trials of GLP-1 receptor agonists.
- The study examined results for over 59,000 patients and found no difference in rates of suicidal ideation/attempt/completion or self-harm between drug recipients and those receiving placebo.
- These findings do not support previous concerns that GLP-1 agonists might present a heightened suicide risk, as has been associated with bariatric surgery in numerous studies.
GLP-1 receptor agonists have been shown to improve diabetes, reduce cardiovascular events, and cause life-changing weight loss. However, concerns have been raised about increased adverse psychiatric effects—specifically, suicide. Given the exponential increase in the use of these agents, even a slightly heightened risk of this catastrophic outcome could have major clinical impacts.
To investigate that possibility, NYU Langone Health researchers launched the first meta-analysis of suicide and self-harm among patients treated with GLP-1 agonists in randomized, placebo-controlled clinical trials.
“Bariatric surgery has long been the gold standard for treating severe obesity, but studies show a small increase in suicide risk after such procedures,” says preventive cardiologist Sean P. Heffron, MD, who led the study. “If GLP-1 agonists pose a similar risk, that’s important to know—and if they don’t, it could further accelerate the sea change occurring in our approach to treating obesity.”
“Bariatric surgery has long been the gold standard for treating severe obesity, but studies show a small increase in suicide risk. If GLP-1 agonists pose a similar risk, that’s important to know.”
Sean P. Heffron, MD
The study’s results, published in JAMA Psychiatry, suggest that the similarities in outcome between the two approaches do not include that potential downside.
Suicide Risk with Bariatric Surgery Raises Concerns About GLP-1
Questions about a link between suicidality and GLP-1 agonists first came to public awareness in July 2023, when the Icelandic national health department described three patients taking the drugs, two of whom had suicidal thoughts and one who engaged in self-harm. That news spurred the European Medicines Agency (EMA) and researchers worldwide to investigate the possibility of a causal connection.
Dr. Heffron and his team, however, had begun their study a year earlier. His curiosity was sparked by a 2022 journal discussion with colleagues in NYU Langone’s Center for the Prevention of Cardiovascular Disease—one of the largest and longest-standing such centers in the country. The group was reviewing a paper on tirzepatide, a GLP-1 agonist, which reported that the drug’s efficacy for weight loss was nearly comparable to that of bariatric surgery.
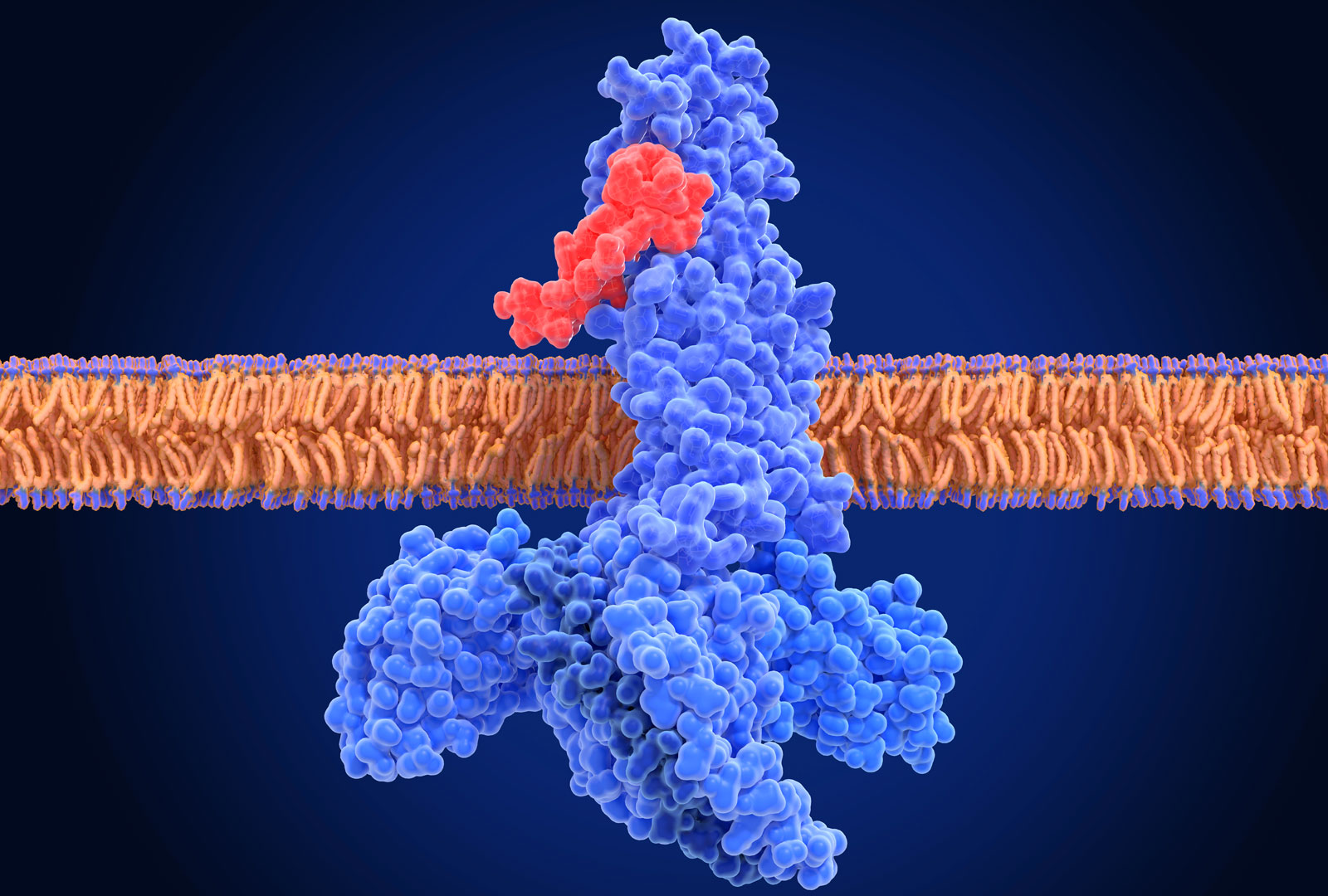
“Why bariatric surgery is so effective is not completely understood,” Dr. Heffron explains, “but we know that it leads, at least transiently, to a rise in blood levels of GLP-1. We also know there are GLP-1 receptors in the brain.” That made him wonder: Is the increase in GLP-1 responsible for the heightened risk of suicide associated with the surgery? If so, he thought, an elevated risk might also be seen with GLP-1 receptor agonists.
Dr. Heffron was among the first cardiologists in the United States to prescribe such drugs—originally intended for those with diabetes—to treat obesity. Although none of his own patients had shown signs of suicidality, he felt it was urgent to learn whether the medications could have that unintended consequence.
To find out, Dr. Heffron and his team began with a comprehensive literature search for randomized, controlled trials involving adults with obesity or diabetes or both treated with GLP-1 agonists for at least six months. The 11 researchers screened over 7,000 articles and extracted data for 144 that met the initial criteria for inclusion.
After querying all available data sources, including direct contact with principal investigators or corresponding authors, the team found that 27 of the trials had recorded risk of adverse psychiatric outcomes. A random-effects meta-analysis of these studies was performed to estimate risk ratios for the primary outcome: suicidal ideation/attempt/completion or self-harm.
Extensive Analysis Brings Reassuring News
By the time this laborious process was completed, the EMA and the U.S. Food and Drug Administration had issued their own preliminary reports, based on analyses of electronic medical records as well as observational studies and clinical trials, which found no link between GLP-1 agonists and suicidal thoughts or self-harm. Both agencies, however, called for further research to determine whether a small risk might exist for some subgroups.
The NYU Langone team’s meta-analysis confirmed and broadened these findings. Across the studies that were included, over 32,000 subjects received GLP-1 agonists and over 27,000 received placebo. The event rate was very low—and statistically comparable—for both cohorts: 33 for patients receiving the drugs, and 27 for those in the control groups.
No evidence emerged, moreover, that patients’ psychiatric history had an impact on risk. Although 11 studies (including nearly 6,000 patients) had a history of suicide attempt/depression as exclusion criteria for enrollment, removal of these studies did not affect the overall findings of the meta-analysis.
“We need to continue with Phase 4 observational trials … But it’s reassuring to see that with the highest level of evidence, there’s no signal for concern.”
Dr. Heffron and his colleagues also conducted a subgroup analysis, collecting trials that compared GLP-1 agonists with DPP-4 inhibitors (an older class of diabetes medications), both of which raise blood levels of GLP-1. “There was no difference in suicide risk between drug recipients and controls with either type of medication,” he notes. “So it would seem that GLP-1 is not the mechanism of the increased risk seen with bariatric surgery.”
The takeaway, Dr. Heffron adds, is that GLP-1 agonists could offer the benefits of bariatric surgery without that elevated risk. “We need to continue with Phase 4 observational trials to look for any rare side effects,” he says. “But it’s reassuring to see that with the highest level of evidence, there’s no signal for concern.”