While neovascular age-related macular degeneration (nAMD) only represents 10 to 15 percent of AMD cases, it was responsible for 90 percent of AMD-related visual impairment before the introduction of injectable anti-vascular endothelial growth factor (VEGF) agents. However, increasing use of these agents contributes significantly to Medicare Part B costs, and frequent (e.g., monthly) intravitreal injections can cause problems for some patients, due to factors such as location, drug access, health literacy, and fear of injections.
In 2022, the U.S. Food and Drug Administration approved the first port delivery system (PDS) with sustained delivery of ranibizumab through implantation, which requires initial surgery with office refills as often as every 6 months.
“The negative aspect of intravitreal injections is that they need to be administered roughly every 1 to 3 months, depending on the patient,” says Ravi S. Parikh, MD, MPH, retina specialist and director of healthcare delivery research for the Department of Ophthalmology. “The purpose of this new device is to act as a drug reservoir, which is surgically implanted into the eye and refilled every 6 months or longer.”
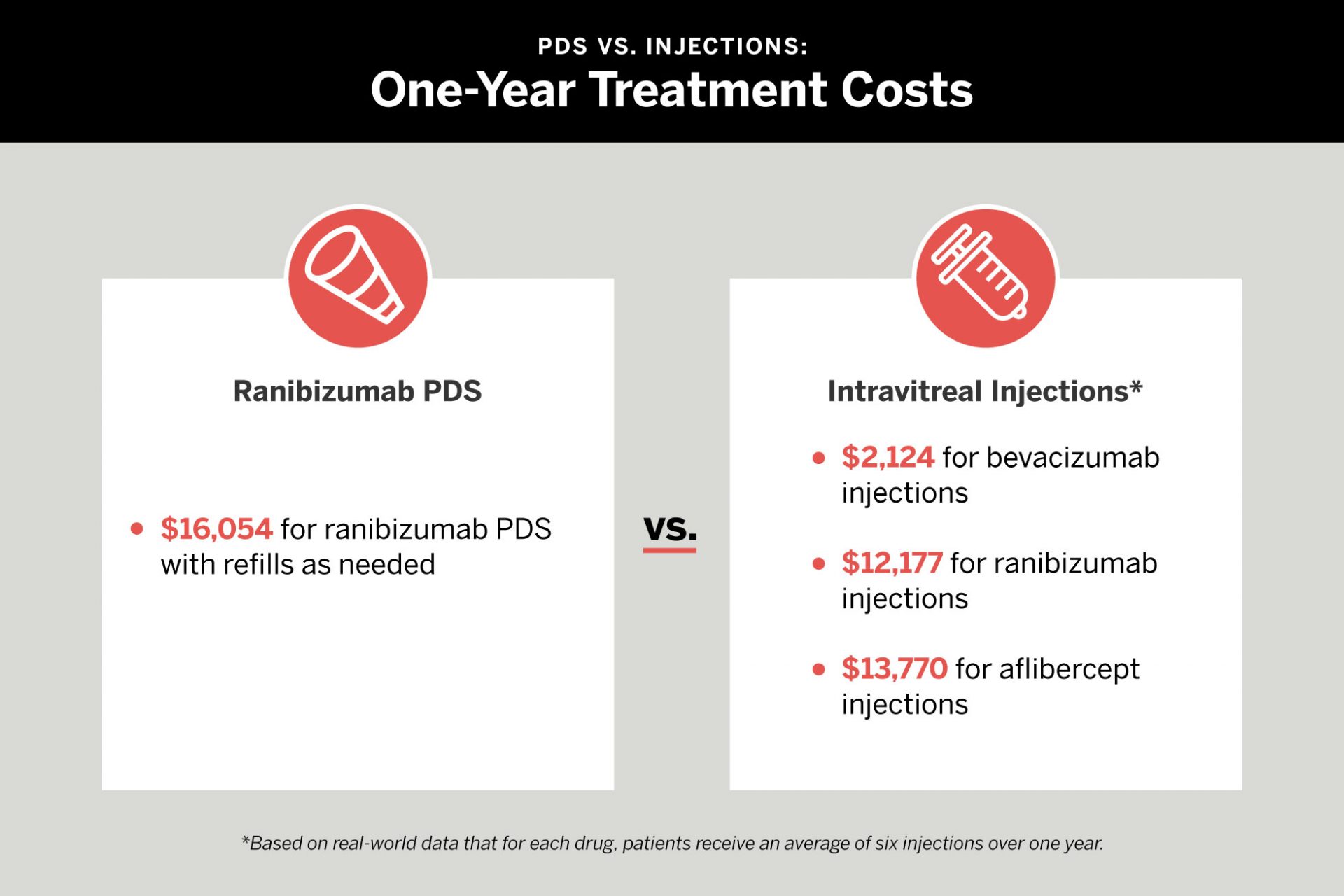
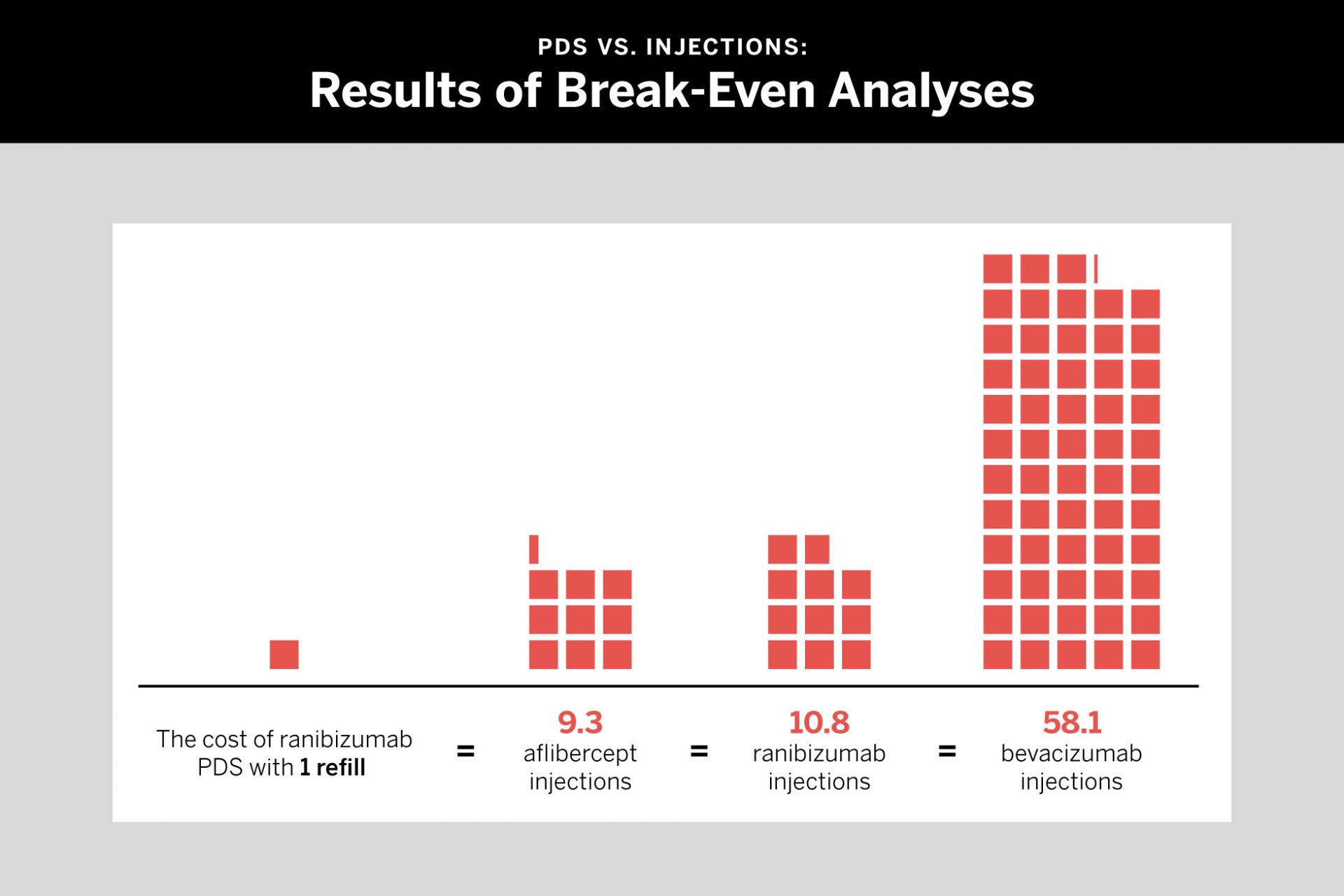
A recent study in JAMA Ophthalmology led by Dr. Parikh and colleagues at NYU Langone Health investigated costs of intravitreal anti-VEGF injections versus ranibizumab PDS for patients with nAMD. The team found that in most clinical scenarios, ranibizumab PDS costs more than bevacizumab in all scenarios studied. For ranibizumab and aflibercept injections, ranibizumab PDS may confer cost savings if monthly injection regimens are required. Yet real-world data suggest bimonthly regimens are more common.
“Based on our findings, for most patients, the best course of action for patient safety, practicality for monitoring, and cost is to continue the current paradigm of coming into the office to receive injections.”
Ravi S. Parikh, MD, MPH
“Based on our findings, for most patients, the best course of action for patient safety, practicality for monitoring, and cost is to continue the current paradigm of coming into the office to receive injections,” Dr. Parikh adds. “For patients who are home bound, live in rural areas, have access issues, or no family support, the PDS system may be a good option, but what is best for patients is to still be monitored regularly, which for now requires in-person visits.”
Disclosure: Dr. Parikh has received consulting fees from Anthem Blue Cross Blue Shield and Apellis Pharmaceuticals.