Vulvovaginal disorders, including vulvar pain, chronic vulvovaginal itching or irritation, and skin conditions such as lichen sclerosus and lichen simplex chronicus, occur frequently and are a major reason many women seek healthcare.
About one-third of vulvovaginal disorders are gynecologic in nature, one-third are dermatologic, and the remaining are undiagnosed vulvovaginitis, says Rebecca G. Podolsky, MD, a general gynecologist and director of NYU Langone Health’s Center for Vulvar Health.
“These conditions can be challenging and time-consuming to diagnose and treat. Patients often see multiple doctors before they receive a diagnosis and treatment plan.”
“The Center for Vulvar Health provides comprehensive and thorough care in this often-overlooked area.”
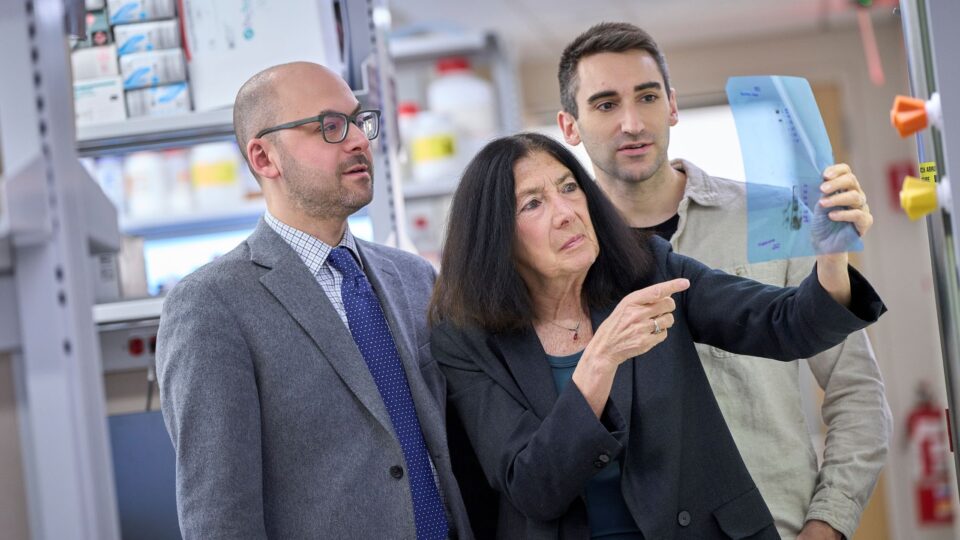
Rebecca G. Podolsky, MD
Gynecologists often receive limited training in the diagnosis and management of vulvar conditions, Dr. Podolsky says. These disorders can also be underrecognized by dermatologists, who may lack comfort with examination techniques and be unfamiliar with normal anatomic variations.
Additionally, many of these conditions are not resolved in one or two visits, making them challenging to manage in a general gynecologic practice, Dr. Podolsky adds.
“The Center for Vulvar Health provides comprehensive and thorough care in this often-overlooked area.”
Recognizing Vulvar Pain
Vulvar pain, or vulvodynia, is a common condition seen at the Center for Vulvar Health. For years, patients with vulvar pain have dealt with uncertain diagnoses and little in the way of treatment, Dr. Podolsky says. “That’s starting to change—there’s more recognition of the problem now.”
“Chronic vulvar pain is prevalent and has a significant impact on quality of life, including sexual function,” she adds. “It can be a very frustrating condition for the patient since the causes are multifactorial and they have usually been told nothing is wrong because their skin looks normal.”
The pathophysiology of vulvar pain is difficult to determine and can be infectious, inflammatory, or neuropathic in nature, Dr. Podolsky says.
A diagnosis requires careful listening to the patient’s symptoms, a focused physical examination, and attention to the common comorbidities (medical and sexual) with which vulvar pain can be associated.
“It can be a long process untangling the causes and finding the right treatments.”
Possible treatment options include topical or oral medications, injections, physical therapy, lifestyle interventions, and surgical procedures.
“It can be a long process untangling the causes and finding the right treatments,” Dr. Podolsky notes.
New Treatments for Vaginal Infections
Dr. Podolsky sees numerous patients with vulvovaginal symptoms caused by yeast or bacteria. About 75 percent of women in the United States develop a vaginal yeast infection, or candidiasis, during their lifetime.
“While many of these conditions are easily treated and resolved, some patients have recurrent or treatment-resistant vulvovaginitis,” Dr. Podolsky says. “Now we have new tools in the arsenal, including Brexafemme (ibrexafungerp), the first new antifungal to be FDA-approved in over 20 years for recurrent yeast infections.”
Vulvar Skin Conditions and Cancer
The Center for Vulvar Health also treats several skin conditions that often affect the vulva, such as lichen sclerosus and lichen planus. Both are inflammatory autoimmune diseases that confer an increased risk for squamous cell carcinoma of the vulva.
It is important for those affected to be on long-term treatment and have regular examinations to keep the disorder under control, prevent or treat symptoms, and lower the risk for developing cancer, Dr. Podolsky notes.
She recommends that gynecologists and dermatologists examine the vulva carefully, empower patients to discuss complaints, “and make use of resources like our center.”