In the early months of the COVID-19 pandemic, clinicians anticipated that many patients who were hospitalized or who had more severe disease might experience the lingering symptoms of a chronic pulmonary disease.
“What we found is that other patients who had mild or even asymptomatic disease, weeks to months later, were also developing symptoms like shortness of breath, fatigue, dizziness, and brain fog,” says pulmonologist Rany Condos, MD, director of NYU Langone Health’s Post-COVID Care Program.
Estimates suggest that roughly 50 percent of patients who’ve had COVID-19 will develop post-acute sequelae of SARS-CoV-2 infection (PASC), or long COVID. “What we are finding in the clinic is that there continues to be an enormous need,” Dr. Condos says.
“It’s not a single disease, and it may turn out that there are multiple causal processes.”
Steven Abramson, MD
To better understand the genetic and immunoinflammatory drivers and other risk factors for PASC that may point toward therapeutic targets and strategies, Dr. Condos and rheumatologist Steven Abramson, MD, are leading a $4.2 million NIH-funded study to characterize the patients in the program.
“While the syndrome is occurring in a substantial number of people, we don’t really understand the pathophysiology or the disease mechanisms,” says Dr. Abramson, chair of the Department of Medicine. “It’s not a single disease, and it may turn out that there are multiple causal processes.”
A Long-Term Assessment of Outcomes
The study will enroll more than 1,200 patients divided into three groups: one with long-term pulmonary symptoms, a second with symptoms that do not include pulmonary complaints, and a third group who have had COVID-19 but no long-lasting symptoms.
“We need to make sure that we’re listening to what patients are telling us, taking that to heart, and adjusting as we go along to make sure that we collect as good a set of data as possible.”
Rany Condos, MD
Beyond characterizing patients’ pulmonary and neurological symptoms and medical history, the study will assess their anxiety, ability to perform daily tasks, and social determinants of health. “We need to make sure that we’re listening to what patients are telling us, taking that to heart, and adjusting as we go along to make sure that we collect as good a set of data as possible,” Dr. Condos says.
Collecting the data over two to four years may provide critical information about the effects of SARS-CoV-2 infection in distinct PASC groups. “Since there’s really no specific treatment to speak of the other purpose of the grant is to understand mechanisms, whether broadly speaking or for each of the different PASC subtypes, to identify targeted treatment approaches,” Dr. Abramson says.
Searching for Genetic and Immunological Triggers
A better understanding of those disease mechanisms may come from determining the inflammatory, immunological, genetic, and autoimmune processes driving the clinical manifestations of PASC.
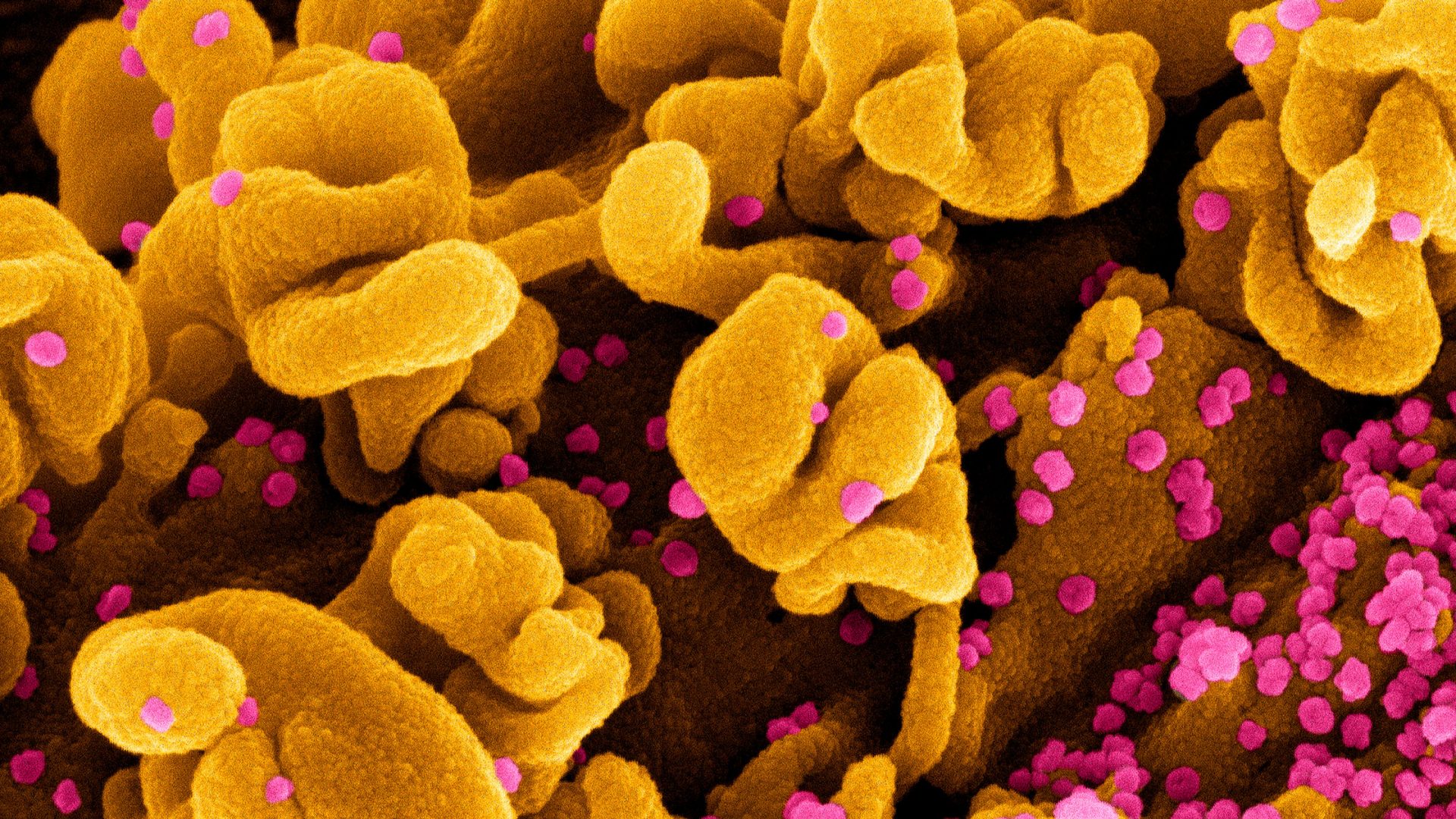
In acutely hospitalized patients with severe COVID-19, the virus somehow activates a cytokine-mediated, host-induced inflammation that can damage multiple organs.
Dr. Abramson and colleagues report on the preprint server medRxiv that variants of the IL1RN gene seem to confer protection against severe disease. Among patients with PASC, the investigators hope to determine whether cytokine levels are persistently elevated, whether autoantibody responses have proliferated, and whether continued inflammation is more associated with a pro-inflammatory genotype of IL1RN.
A whole genome sequencing analysis of each patient will aid the search for other candidate genes that increase the susceptibility or severity of PASC.
“Even though we know there is persistent inflammation in some of these patients, we don’t know why,” Dr. Abramson says. The study may shed new light on whether a virus-induced autoimmune response or the persistence of viral particles in the gut or elsewhere drives the disease in some patients.
Sifting Through Potential Risk Factors
The researchers will also examine how genetic variants linked to PASC susceptibility and severity may vary across self-identified race and ethnicity. Some genetic polymorphisms, for example, may modulate immune–inflammatory responses that influence the incidence or severity of PASC syndromes in certain patient groups.
“We’re trying to be very consistent, organized, and defined in terms of how we’re evaluating these patients because we’re dealing with something that has not been defined until now,” Dr. Condos says.
In effect, Dr. Abramson adds, the study is an extension of the integrated clinical program that evaluates and cares for patients through the close coordination of pulmonologists, neurologists, rheumatologists, and specialists at NYU Langone’s Rusk Rehabilitation, among others.
“I think what we are offering people is some assurance that we can at least help diagnose a problem and provide supportive therapy,” he says. “That’s really important to people, otherwise they feel like it’s just in their head.”