Physicians and speech-language pathologists in NYU Langone’s Voice Center are participating in multiple studies aimed at determining the elusive causes and mechanisms of dysphagia and finding improved methods for predicting and diagnosing the disorder.
A one-year pilot study—a multidisciplinary collaboration with the Spine Center, Rusk Rehabilitation, and the Department of Communicative Sciences and Disorders at NYU Steinhardt—is investigating long-term dysphagia and dysphonia in patients who have anterior cervical discectomy and fusion (ACDF) spine surgery.
A particular challenge to understanding the prevalence and pathophysiology of dysphagia post-ACDF is distinguishing a short-term impairment caused by post-surgical edema from a more serious long-term iatrogenic injury to the swallowing nerves and muscles at risk during the surgery, says Matina Balou, PhD, a clinical assistant professor of otolaryngology-head neck surgery.
Expected Edema vs. Atypical Swallowing
Postsurgical edema alone typically resolves in the first few months, Dr. Balou says. Patients who are still experiencing dysphagia after that time are referred to speech-language pathology for a swallow evaluation.
“Currently, by the time patients come to us with symptoms, they have already suffered for several months,” says Dr. Balou. “If we can identify an algorithm that would let surgeons know a patient is high-risk for long-term problems, we could recognize what’s happening and intervene at patients’ first complaint—potentially restoring their quality of life sooner.”
After reviewing approximately 2,000 articles, the researchers found that nearly half of studies that described the problem of dysphagia after ACDF utilized the Bazaz scale, a simple, two-question, patient-reported measure.
“If we can identify an algorithm that would let surgeons know a patient is high-risk for long-term problems, we could recognize what’s happening and intervene at patients’ first complaint—potentially restoring their quality of life sooner.”
Matina Balou, PhD
“This is a multifactorial problem that demands more than a yes/no analysis,” says Dr. Balou. “Most patients say they have swallowing issues post-surgery, but it doesn’t necessarily translate into weakness or destruction.”
Identifying Predictive Measures
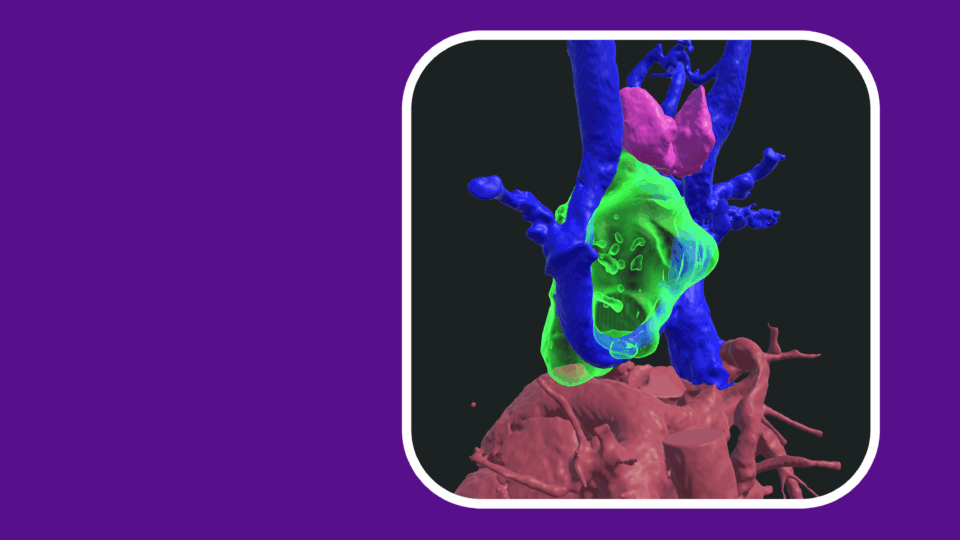
Working with a group of neurosurgeons led by Anthony K. Frempong-Boadu, MD, co-director of the Spine Center, the pilot study will follow 20 patients through their ACDF surgery and recovery. Participants are examined through two visits at the Voice Center—six weeks pre-ACDF and six weeks post-ACDF—with the research team conducting three primary evaluations: a videofluoroscopic swallow study (VFSS), measures of pharyngeal edema using an acoustic pharyngometer, and an acoustic voice sample. Additionally, the researchers administer pre-and post-surgery questionnaires.
“We are one of the only centers that has the videofluoroscopy equipment on site, which makes it easier for patients to participate in our research,” Dr. Balou notes.
Of seven participants who have currently completed their surgeries, three have had to enroll in swallowing therapy pre-op to improve safety and efficacy.
The team hopes to determine whether acoustic pharyngometer and voice sample can be validated as accurate noninvasive measures of edema, data that will pave the way toward a future multicenter research study. An additional goal is to describe the physiology of swallowing post-ACDF, uncovering data that could predict which patients might experience long-term impairment.
Expanding Dysphagia Evaluation
Voice Center researchers are also using videofluoroscopy, high-resolution manometry, and other advanced imaging to establish predictive measures for dysphagia caused by conditions such as stroke, pulmonary disease, head and neck cancer, spinal cord injury, and aging. Dr. Balou describes a portfolio of ongoing studies.
One study seeks to determine if swallowing problems can be predicted in the ENT office setting using findings on flexible laryngoscopy prior to gold standard VFSS/endoscopic swallow evaluation. A separate longitudinal study is evaluating dysphagia in pulmonary patients with non-tuberculous mycobacteria. Another observational study has reviewed phenotypes of the epiglottis to collect classification data for creating a dysphagia prediction system.
“It’s difficult to tease apart which part of the throat is not doing what it’s supposed to do,” Dr. Balou says. “The truth is that we do multiple swallowing evaluations every day and prescribe exercises that work. What we are lacking is treatment studies—there’s a gap in the literature. But we are improving patients, I see it every day.”