In a retrospective study of more than 20,000 patients undergoing total knee or hip arthroplasty, NYU Langone Health researchers reported the first validated decision-making tool that predicts discharge to home versus inpatient rehabilitation or a skilled nursing facility.
Within bundled payment models for total joint arthroplasty, costs are higher for discharge to rehabilitation or a skilled nursing facility, but that level of care is often necessary for better patient recovery. “Sometimes, our patients are not physically or mentally ready to go home alone and take care of themselves,” says orthopedic surgeon and senior study author Ran Schwarzkopf, MD. “They need some environment to care for them until they’re able to do that.”
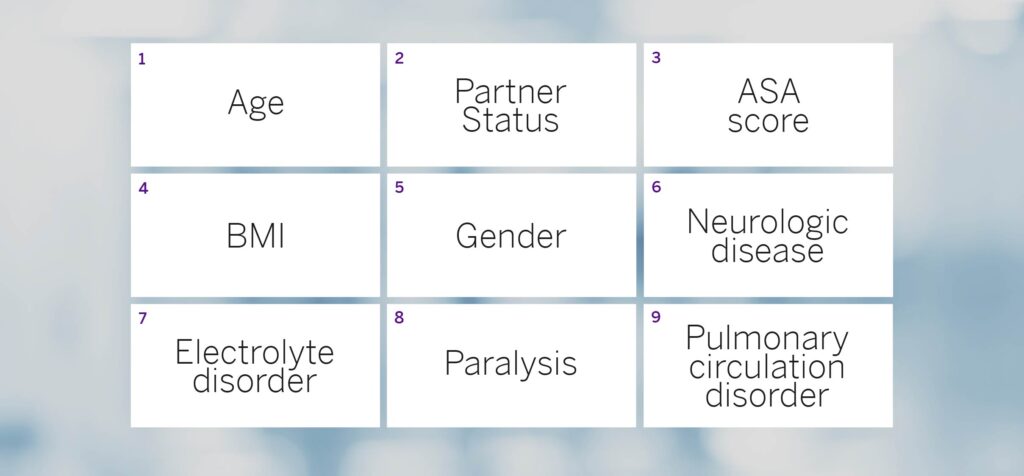
Dr. Schwarzkopf led a group of colleagues from across the nation in developing an online prediction model consisting of nine preoperative parameters to identify high-risk patients (Figure 1). The focus on parameters easily pulled from the electronic medical record enables discharge planning to occur well in advance of surgery.
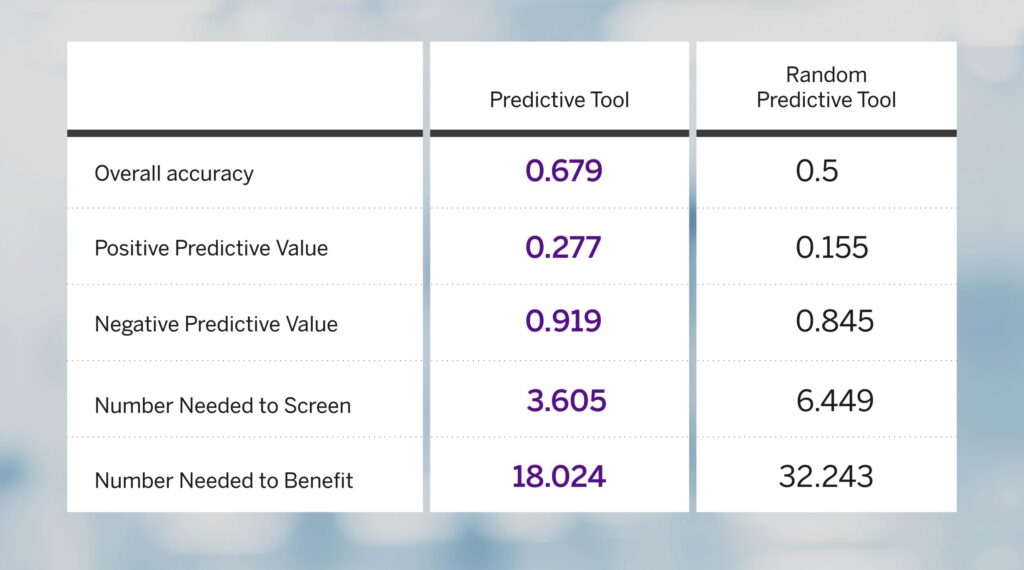
Compared to simple random selection, the clinical decision-making tool yielded a 79 percent improvement in positive predictive value and a 56 percent decrease in the number needed to screen to identify 1 true positive (Figure 2).
The study also indicated that 15.5 percent of the patients qualified for rehabilitation, which Dr. Schwarzkopf notes is to be expected for a tertiary referral center that often sees patients with comorbidities.
“Not only does it help a patient meet expectations and prepare, it also helps the family or caregivers.”
Ran Schwarzkopf, MD
The tool, he says, merits consideration for clinical use because of its value for patient counseling, preoperative optimization, and discharge planning. “Not only does it help a patient meet expectations and prepare, it also helps the family or caregivers,” he says. “In addition, it helps the system prepare better for where to do the surgery and what to expect for the patient after the surgery.”






