Referral Notes:
- An NYU Langone Health study found that peripheral ischemia accelerates breast cancer progression, with mice exposed to hind-leg ischemia showing double the tumor growth of controls.
- Tumor suppression was impaired by a shift from lymphoid to immunosuppressive myeloid cells in the tumor microenvironment and bone marrow—a proinflammatory phenotype linked to aging of the hematopoietic niche.
- The findings suggest new approaches to cancer prevention and treatment that counter the tumor-promoting effects of ischemic injury.
Patients with cardiovascular disease have an increased risk of developing cancer, and the reverse is also true. Evidence increasingly suggests these diseases share pathophysiological mechanisms that result in bidirectional health impacts, but the intricacies of this relationship are only beginning to be understood.
A study led by NYU Langone Health researchers sheds light on one side of the equation—how cardiovascular dysfunction contributes to tumor progression. The paper, published in JACC: CardioOncology, suggests that peripheral ischemic injury drives nascent tumor growth via accelerated hematopoietic aging.
“Our study shows that impaired blood flow drives cancer growth regardless of where it happens in the body.”
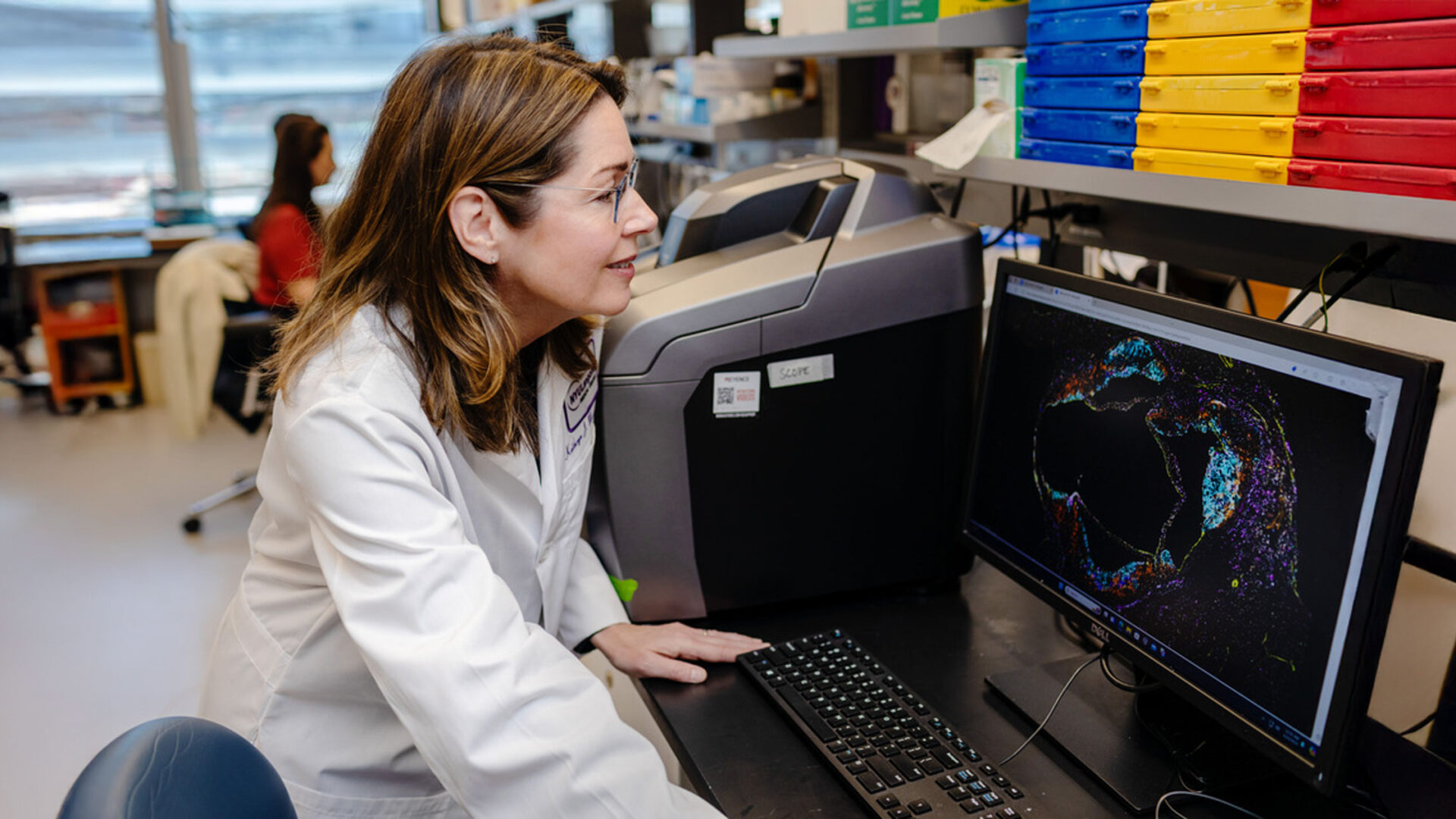
Kathryn J. Moore, PhD
“Our study shows that impaired blood flow drives cancer growth regardless of where it happens in the body,” says corresponding author Kathryn J. Moore, PhD. “In addition, we’ve identified key immune-mediated pathways by which this process takes place.”
Peripheral Ischemia Doubles Tumor Growth
The study builds on earlier research by Dr. Moore and colleagues, which showed that ischemia associated with myocardial infarction (MI) accelerates breast cancer tumor growth in a mouse model by reprogramming hematopoietic cells in bone marrow to be more immunosuppressive.
In the new study, the team set out to learn whether peripheral artery disease (PAD) could produce similar results. In the experimental group, mice were injected with mammary tumor cells either before or after ischemia was induced surgically in one hind leg to simulate PAD. A control group underwent sham surgery.
Breast tumors grew at double the rate in the hind-leg ischemic (HLI) mice than in controls, whether tumor injection occurred before or after HLI. “These results were similar to what was observed after coronary ligation in a mouse model of MI, suggesting that peripheral ischemia, like cardiac ischemia, robustly accelerates tumor growth,” says Dr. Moore.
Shift in Immune Cells Weakens Defenses
To understand how peripheral ischemia presses the accelerator, the team first examined the tumor immune microenvironment in HLI-experienced mice. As with cardiac ischemia in the earlier study, there were shifts toward immune cells that cannot effectively fight cancer.
Within the tumors of these mice, the researchers observed higher proportions of myeloid cells—including immunosuppressive monocytes, macrophages, and neutrophils—than in control animals. (Among lymphoid cells, only immunosuppressive regulatory T cells were elevated.) Such alterations were observed whether HLI occurred after or before tumor injection.
A similar shift toward myeloid cells at the expense of tumor-fighting lymphoid cells was seen in the blood of the HLI-experienced mice—a change correlated with poor clinical outcomes in a variety of cancers. The researchers determined that peripheral ischemia, like cardiac ischemia, prompts the preferential release of myeloid cells from bone marrow.
“Our findings underscore the critical importance of addressing metabolic and vascular risk factors as part of a comprehensive cancer prevention strategy.”
Further analysis showed that myeloid progenitor cells carrying a proinflammatory program were predominant. “All these changes add up to a phenotype associated with aging of the hematopoietic niche,” says Dr. Moore.
Epigenetic Changes Exacerbate the Damage
To uncover the regulatory mechanisms driving ischemia-induced myeloid bias, the team conducted a multiomic, single-nucleus study of chromatin accessibility and gene expression. They found that HLI not only altered the expression of hundreds of genes but also reorganized the structure of chromatin—a change that impeded immune cells’ ability to activate genes necessary for cancer defense.
“We revealed that peripheral ischemia leads to epigenetic reprogramming of bone marrow progenitors that induces both immediate and long-term changes in antitumoral immune responses,” Dr. Moore says.
Integrating Cardiology into Cancer Care
These insights on the links between cardiovascular disease and cancer point toward cross-disciplinary clinical approaches, she adds.
“Our findings underscore the critical importance of addressing metabolic and vascular risk factors as part of a comprehensive cancer treatment strategy. They also suggest new preventive and therapeutic strategies, such as earlier cancer screening for patients with peripheral artery disease and using inflammation-modulating therapies to counter the tumor-promoting effects of ischemic injury.”