Referral Notes:
- One of that nation’s few comprehensive centers for pediatric MS and related disorders, NYU Langone offers rapid, multidisciplinary care—including expert off-label use of adult-approved therapies.
- Supported by three pediatric MS specialists, the center provides consults for suspected neuroimmune cases within 24 to 48 hours.
- Integrated mental health, social work, neuropsychology, and academic support help children and families manage chronic illness and pursue full, independent lives.
NYU Langone Health is home to one of the nation’s most comprehensive centers for the evaluation and management of pediatric multiple sclerosis (MS) and related neuroimmune disorders. The program is led by internationally recognized MS expert Lauren B. Krupp, MD, and pediatric neuroimmunologists Kimberly A. O’Neill, MD, and Lena H. Bell, MD.
Together, the team delivers a multidisciplinary, high-acuity approach to diagnosing and managing pediatric-onset MS, myelin oligodendrocyte glycoprotein antibody-associated disorder (MOGAD), neuromyelitis optica spectrum disorder (NMOSD), and other rare inflammatory disorders of the central nervous system.
“The level of subspecialty focus we offer as an inpatient neuroimmunology service does not exist elsewhere in the New York City region,” says Dr. Krupp. “It is rare to find a center with even one pediatric MS specialist, while we offer three—plus a supportive team of experts in a true multidisciplinary model.”
Closing the Gap in Pediatric MS Care
The service was designed to address a long-standing gap in pediatric neuroimmunology. Historically, pediatric MS cases were often bounced between pediatric and adult neurology, with no clear path to diagnosis or disease-modifying therapy. Dr. Krupp, who established the first dedicated pediatric MS center in the U.S. in 2002 and later founded the International Pediatric MS Study Group, notes that the field has evolved in response to emerging therapies.
“With the advent of disease-modifying treatments in the 1990s, accurate and timely diagnosis in children became critical,” she says. “We now know that early intervention significantly alters long-term outcomes.”
“It is rare to find a center with even one pediatric MS specialist, while we offer three.”
Lauren B. Krupp, MD
In spring 2024, NYU Langone formalized a consult pathway for inpatient pediatric and adult neurology services to rapidly access subspecialty input for suspected neuroimmune cases. Consults are triaged by a dedicated fellow and evaluated by faculty within 24 to 48 hours.
The clinic’s reach is increasingly regional, drawing referrals from across New York, New Jersey, Connecticut, and beyond—including recent cases from Boston, North Carolina, and Puerto Rico.
One early consult involved a five-year-old child with persistent dysphagia following presumed post-viral brainstem encephalitis. After first-line treatments failed, the pediatric neuroimmunology team was consulted and recommended plasma exchange. The child subsequently recovered full swallowing function and avoided percutaneous endoscopic gastronomy (PEG) tube placement.
“That case highlighted exactly why this service is needed,” says Dr. O’Neill. “It’s not uncommon for immune-mediated pathology to be under-recognized or for escalation of care to be delayed in the absence of neuroimmunology consultation.”
Expertise Across the Neuroimmune Spectrum
In addition to the inpatient service, the team sees patients in the outpatient clinic once per week, together reviewing every case before each patient is seen. The clinic sees a diverse population of children with demyelinating disease. Among children under age 11, the majority of cases are ultimately diagnosed with MOGAD, while adolescents more commonly present with MS. A smaller percentage of patients across age groups are diagnosed with NMOSD.

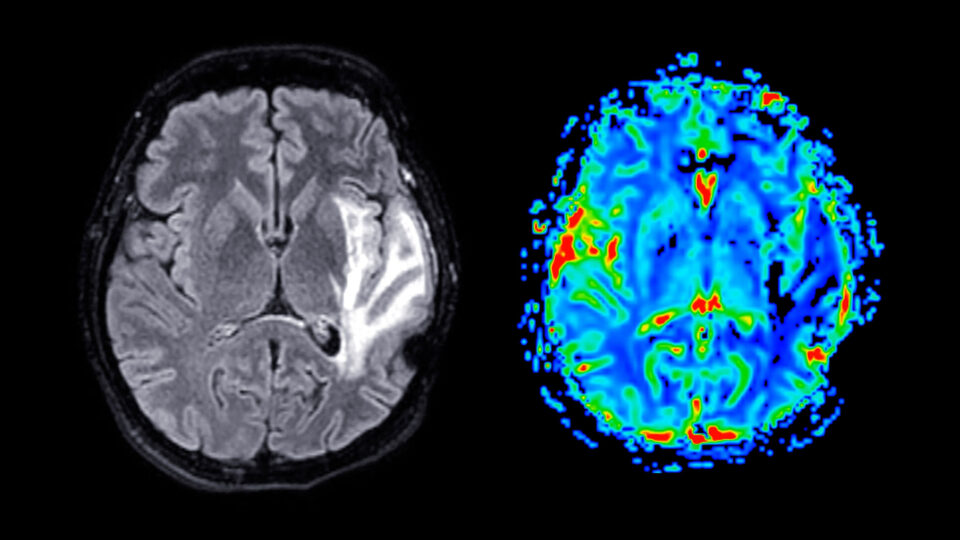
Symptom overlap between these conditions is significant—most commonly optic neuritis, transverse myelitis, hemiparesis, and balance problems—though each condition comes with nuances identified through clinical and radiologic distinctions, combined with serum and cerebrospinal fluid biomarkers. For example, MOGAD and NMOSD tend to be associated with long lesions on spinal cord imaging, while MS is associated with shorter, multiple lesion segments.
“Our ability to parse those presentations with imaging, antibody testing, and clinical context is critical—and that process always starts with a very thorough clinical history from the patient and the family,” explains Dr. O’Neill.
Treatment Limitations—and Advocacy
Despite over 20 FDA-approved MS therapies for adults, only one—fingolimod—has pediatric approval. NYU Langone’s team routinely uses off-label therapies supported by adult data, advocating with insurers and participating in national efforts to close the regulatory gap.
“We personalize treatment plans based on clinical course, imaging, and lab surveillance,” says Dr. Krupp. “But the disparity in access remains a challenge. It can take years for pediatric approvals to follow adult indications—even when the mechanisms of action and risk-benefit profiles are comparable.”
For this reason, the team does not routinely enroll pediatric patients in randomized trials when superior therapies are already accessible through off-label prescribing. Rather, research by Drs. Krupp, O’Neill, and Bell is focused on following patients’ long-term outcomes in order to optimize treatment protocols, along with characterizing risk factors for disease relapse.
“These advances in medical knowledge are leading to excellent outcomes—often in situations where in the past there was much uncertainty.”
Lena H. Bell, MD
“The rate of progress for pediatric neuroimmunology is astounding, as each year our understanding and the availability of effective therapies have greatly increased,” says Dr. Bell. “These advances in medical knowledge are leading to excellent outcomes—often in situations where in the past there was much uncertainty.”
Comprehensive, Whole-Child Care
The program integrates mental health care, social work, neuropsychology, and school accommodations into every patient’s care plan. A dedicated nurse practitioner with expertise in behavioral health, as well as a full-time social worker, meet regularly with families to help address the patient and family burden of managing a chronic disease.
The team also coordinates with rheumatology, infectious disease, immunology, and neurogenetics for complex or ambiguous cases.
“It’s not just disease control. We’re supporting patients across all dimensions of chronic illness—academic, emotional, and developmental.”
Kimberly A. O’Neill, MD
“It’s not just disease control,” says Dr. O’Neill. “We’re supporting patients across all dimensions of chronic illness—academic, emotional, and developmental.”
Longitudinally, most patients diagnosed and treated early for MS and related conditions experience favorable outcomes. Many go on to higher education, employment, and independent adulthood. However, delays in diagnosis, limited treatment access, or comorbid psychosocial challenges can negatively impact trajectory.
“Our oldest patients with pediatric-onset MS are now in their 30s,” says Dr. Krupp. “Many are thriving, but the early years are crucial. Our goal is to intervene aggressively and support them holistically.”