The incidence of pancreatic cysts is rising, and while most are benign, a small percentage have the potential for malignant transformation. In response to growing questions about their evaluation and treatment, internationally renowned pancreatic cancer specialist Tamas A. Gonda, MD, recently co-authored a review in The New England Journal of Medicine on the diagnosis and management of these lesions.
In this interview, Dr. Gonda, director of NYU Langone Health’s Pancreatic Disease Program, breaks down best practices and emerging trends in pancreatic cyst management. He highlights key strategies for assessing malignancy risk and stresses the importance of a multidisciplinary evaluation based on an algorithmic approach.
Physician Focus: What sparked your interest in pancreatic cysts?
Dr. Gonda: My career has focused on the prevention and early detection of pancreatic cancer because I believe this is one of the most effective ways to improve outcomes and survival for this disease.
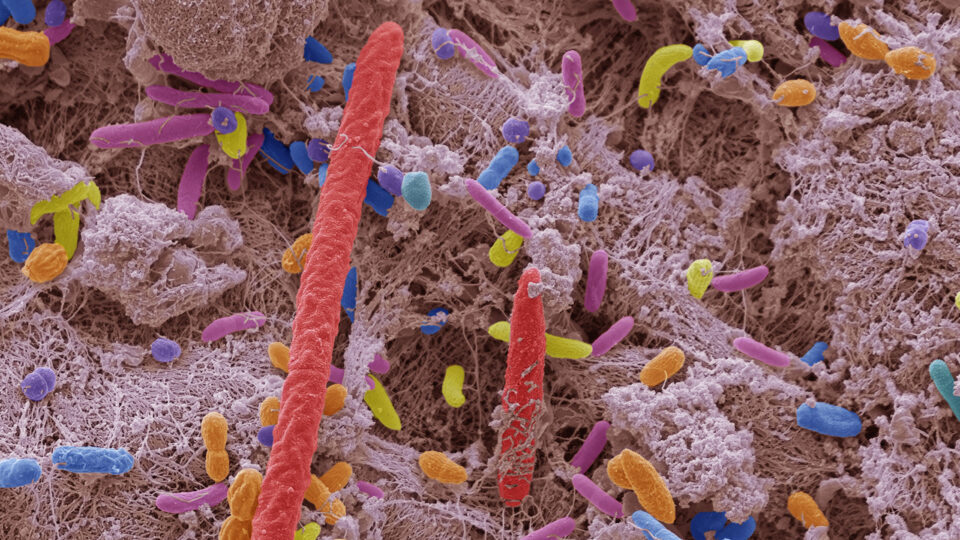
In recent decades, pancreatic cysts have become increasingly recognized as potential precursors to cancer, and these lesions are the only precursors to pancreatic cancer that can be routinely identified on conventional imaging. Therefore, understanding the disease biology and improving diagnosis and treatment with new strategies could have an enormous impact on patients.
“These lesions are the only precursors to pancreatic cancer that can be routinely identified on conventional imaging.”
Tamas A. Gonda, MD
Physician Focus: Pancreatic cysts are often found incidentally on imaging, but only a minority become malignant. How do you assess the risk of malignant transformation?
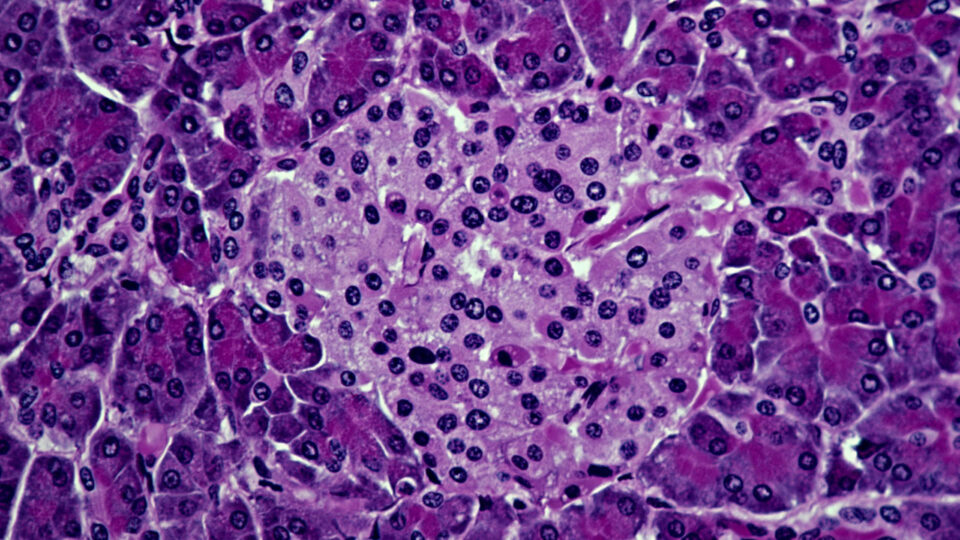
Dr. Gonda: There are more than 20 different types of pancreatic cysts. The two most common premalignant lesions are mucinous cystic neoplasms (MCNs) and intraductal papillary mucinous neoplasms (IPMNs), accounting for about 50 percent of cysts found incidentally on imaging. The risk of malignant transformation is quite variable, ranging from 1 percent to over 80 percent, and depends on a number of cyst and host features. Other types, such as pseudocysts and serous cystadenoma (SCA), are the most common benign lesions.
Our primary goal is to identify the small proportion of cysts that exhibit high malignant potential. This is best done using an algorithm-driven, multidisciplinary approach. Determining the type of cyst is a key first step in risk assessment.
Physician Focus: Noninvasive imaging studies are an important first step in risk assessment. When should secondary imaging modalities, such as endoscopic ultrasonography and fluid aspiration, be considered?
Dr. Gonda: That’s a good question. In some cases, endoscopic ultrasonography can be used to improve risk stratification in patients with intermediate-risk lesions. It can also support the diagnosis of benign or low-risk cysts. For those with high-risk cysts, endoscopic ultrasonography can aid in establishing a preoperative diagnosis of advanced neoplasia.
With regard to fine-needle aspiration of cyst fluid, measurement of glucose levels, amylase, and carcinoembryonic antigen (CEA) can help to confirm the diagnosis of neoplasia—but it is not useful for grade determination. Additionally, DNA isolated from the cyst fluid can aid detection of mutations associated with specific neoplasms, particularly in the context of inconclusive findings.
“Over the next few years, I expect additional molecular markers from the cyst fluid will become a routine part of cyst evaluation.”
Current evidence increasingly favors the integration of DNA-based mutational analysis in the diagnostic evaluation of pancreatic cysts. Mutational status can provide useful information about the risk of advanced neoplasia, especially in the absence of cytologic abnormalities. Over the next few years, I expect additional molecular markers from the cyst fluid will become a routine part of cyst evaluation. Currently, this is an ongoing area of investigation at our institution.
Physician Focus: Is surgical resection the best option for patients with MCNs and IPMNs?
Dr. Gonda: Not always. Once a definitive or suspected diagnosis of a mucinous cyst has been made, appropriate management may include surgery, routine surveillance, or no intervention at all. Several factors need to be considered when deciding on a treatment plan, including the patient’s overall health, risk of malignant transformation, and risk profile for pancreatic cancer. These factors include family history, germ line genetic profile, and environmental conditions.
Although the guidelines are discordant, most of them recommend that patients with high-risk cysts and an acceptable operative risk profile undergo resection. Minimally invasive surgical techniques are increasingly being adopted, and at experienced centers, such as NYU Langone, the outcomes are comparable or superior to open surgery, with faster recovery time and shorter length of hospital stay.
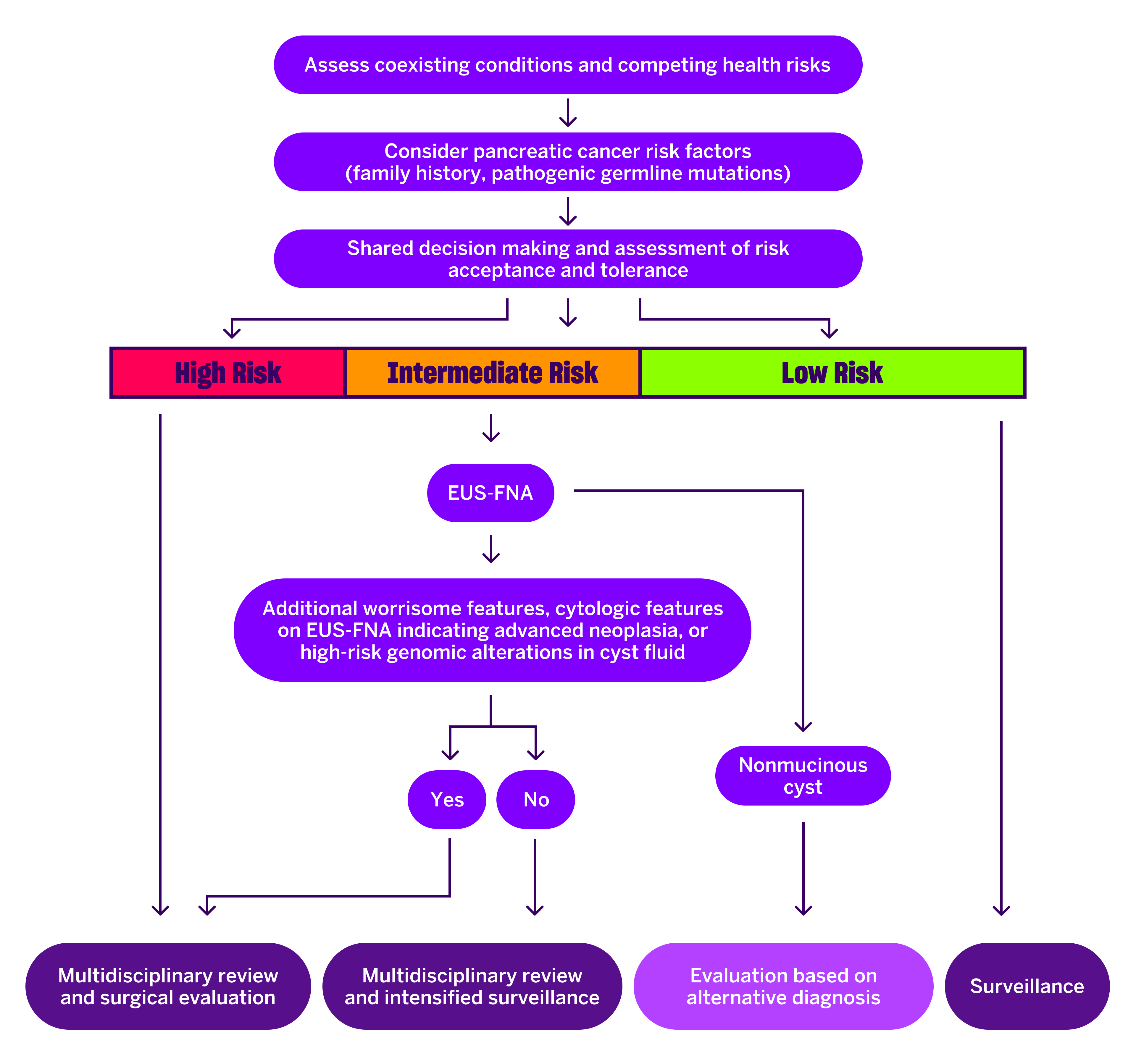
In some instances, it is appropriate to resect intermediate-risk cysts. For these cases, endoscopic ultrasonography and cyst-fluid analysis are especially useful to aid in this decision. The presence of cytologic features indicative of advanced neoplasia or high-risk genomic alterations in the cyst fluid favors surgical intervention, whereas their absence favors surveillance.
In rare cases, low-risk cysts may be appropriate for surgical resection, but surveillance is most common. Notably, current evidence does not unequivocally support surveillance, so when the risk of progression is minimal, cessation of surveillance is also a reasonable option.
Physician Focus: What unmet needs currently exist in the field, and how do you foresee these being addressed in the next three to five years?
Dr. Gonda: Our field lacks long-term prospective data to guide treatment decision-making. Despite only a small proportion of cysts becoming malignant, it’s essential to follow patients over time to inform evidence-based best practices.
“Despite only a small proportion of cysts becoming malignant, it’s essential to follow patients over time to inform evidence-based best practices.”
At NYU Langone, we participate in a number of research collaborations, notably the International Cancer of the Pancreas Screening (CAPS) Consortium and the Pancreatic Cyst Follow-up, an International Collaboration (PACYFIC) study, with the aim of bringing together data from different sites to draw insights about optimal treatment strategies.
Another challenge is the discordance between clinical practice guidelines. To solve this problem, we are working toward a unified global guideline, but this is still a few years away.
In many other areas of cancer prevention, minimally invasive, nonsurgical approaches to treat precancerous lesions have taken hold. I’m optimistic that we will be able to routinely offer different methods of endoscopic ablation of cysts to our patients. Here at NYU Langone, this is one of our areas of investigation and focus.