Controlling the spread of COVID-19 in nursing homes was greatly complicated by asymptomatic carriers, atypical symptoms, and the frequency of close contact between staff and residents. In March 2020, the CDC implemented multiple restrictions in a bid to limit the spread of COVID-19 in those care settings, including restricting all visitors and nonessential personnel and canceling communal dining and group activities.
As part of a larger research effort in New York City nursing homes to improve residents’ sleep/wake patterns, researchers at NYU Langone Health and their collaborators compared changes in nighttime noise before and after implementation of the 2020 COVID-19-related restrictions. Previous research had linked higher noise levels to poor sleep and more behavioral disturbance among residents.
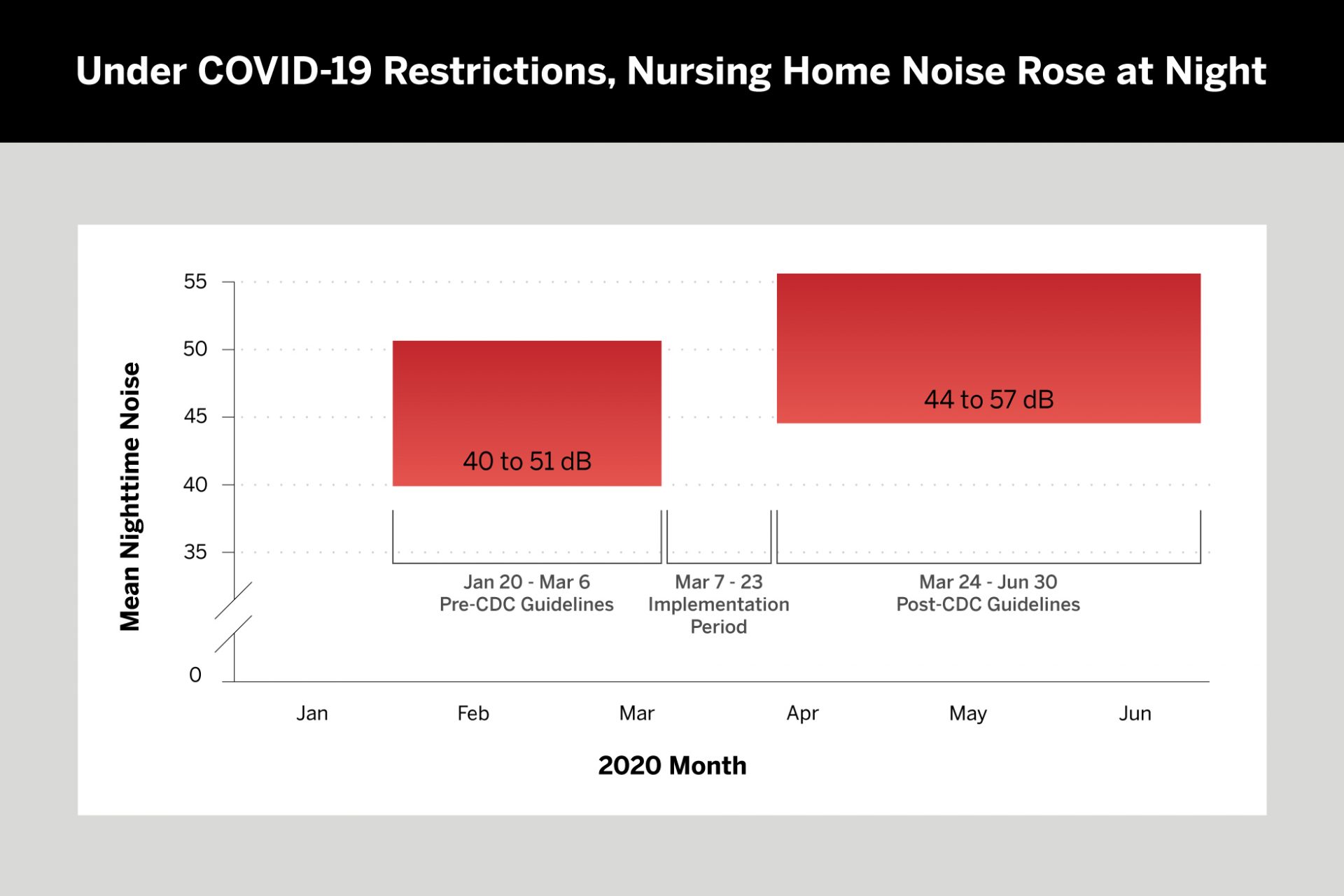
The new study, published in the Journal of the American Medical Directors Association and led by Joshua Chodosh, MD, director of the Division of Geriatrics and Palliative care, found that nighttime noise levels abruptly increased after the CDC-recommended restrictions. Data collected from noise-monitoring devices on six units in two nursing homes showed a significant increase in noise at all locations within one facility and about half of all locations within the second facility. Those changes persisted for months.
Isolation from family and friends, the absence of normal recreational activities, and changes in care providers due to illness of regular staff may have contributed to altered sleep and more noise, says study coauthor and geriatric nursing specialist Abraham A. Brody, PhD. “Simply put, nursing homes were turned on their head. They were struggling to provide care and stay afloat with both residents and staff getting sick.”
“You can’t just attack this problem at one time of day. It takes a concerted holistic effort. Simple environmental modifications can have huge effects on outcomes and our job is to help get that implemented across practice settings nationwide.”
Abraham A. Brody, PhD
Dr. Brody says one lasting lesson is the importance of the 24-hour sleep cycle. “You can’t just attack this problem at one time of day. It takes a concerted holistic effort. Simple environmental modifications can have huge effects on outcomes, and our job is to help get that implemented across practice settings nationwide.”