The global prevalence of non-alcoholic fatty liver disease (NAFLD) is approximately 25 percent, but can rise rapidly in the context of additional risk factors, such as obesity and type 2 diabetes.
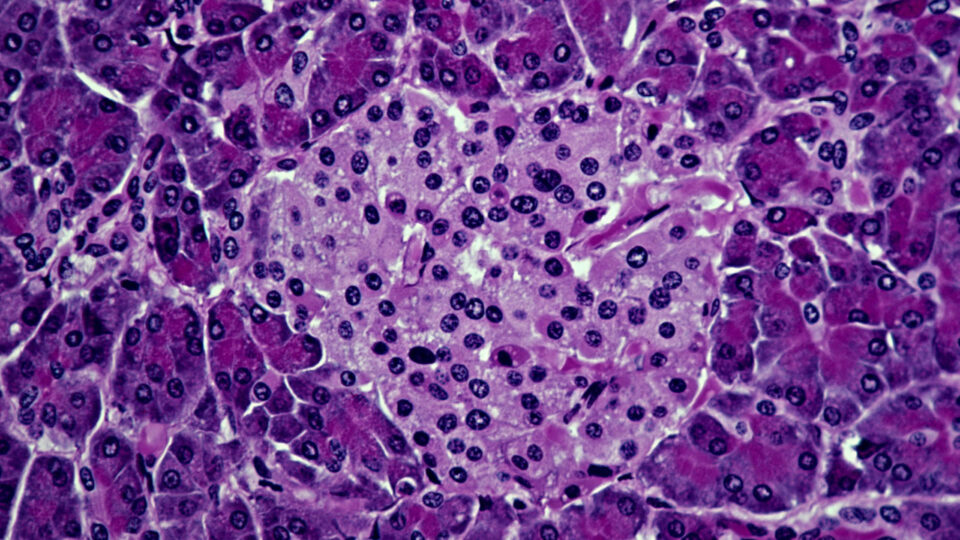
NAFLD can be histologically divided into non-alcoholic fatty liver (isolated hepatic steatosis) and non-alcoholic steatohepatitis (NASH). Research suggests that the stage of liver fibrosis is the most important determinant of patient outcomes and mortality.
“Patients with NASH and advanced hepatic fibrosis are at significant risk for liver-related complications, including hepatocellular carcinoma, end-stage liver disease, and the need for liver transplantation,” says hepatology director Ira M. Jacobson, MD.
For affected patients, Dr. Jacobson describes several strategies that can promote timely diagnosis, plus new treatments on the horizon.
Non-invasive Diagnosis
Non-invasive tests, including blood tests and imaging modalities, have emerged as useful techniques to diagnose and stage NAFLD. Since clinical presentation is often non-specific, patients are not suspected of having liver disease until they develop late stage cirrhosis, Dr. Jacobson says.
“Patients may have had years of minimally elevated alanine aminotransferase levels, that were not recognized as potentially portending progressive liver disease. Only a small proportion of cases are identified in the primary care setting.”
While liver biopsy remains the gold standard in diagnosing and predicting the severity of NAFLD, there are drawbacks including its inherent invasiveness and significant sampling variability.
Among a variety of blood-based parameters, the Fibrosis-4 index (FIB-4) is simple and can be used to diagnose and stage fibrosis. FIB-4 can be easily calculated online in less than a minute using common laboratory findings combined with the patient’s age. It has well established cutoff values for predicting the presence or absence of advanced scarring or cirrhosis, although indeterminate values may occur.
Imaging modalities, such as vibration-controlled transient elastography, supersonic shear imaging, and magnetic resonance elastography can help quantify the degree of scarring, Jacobson says.
“Radiographic evaluation using elastography to determine the degree of fibrosis is based on liver stiffness, a property that is conferred by scar tissue.”
New Drugs
To date, no drugs have been FDA-approved for the treatment of NAFLD, although several are under investigation, with multiple trials ongoing at NYU Langone.
A key goal of pharmalogic therapy is to promote weight loss, particularly in those who fail to achieve their goals through diet and exercise alone. One drug class, glucagon-like peptide 1 (GLP1) agonists, is used extensively in diabetic patients and works in substantial part by inducing weight loss.
“The recent approval of the first GLP1 agonist specifically for weight loss was an important advance,” explains Jacobson. “GLP1 agonists alone or in combination with other agents are being studied for NAFLD in ongoing clinical trials.”
Additional drug classes under investigation include farnesoid X and peroxisome proliferator-activated receptor receptor agonists, FGF19 and FGF21 analogs, and thyroid hormone receptor beta-selective agonists.
“Novel therapies targeting not one, but multiple features of this condition hold great promise.”
Ira M. Jacobson, MD
“Currently, there are over 50 investigational drugs being evaluated in NAFLD,” says Jacobson. “Novel therapies targeting not one, but multiple features of this condition hold great promise.”