Referral Notes:
- NYU Langone is the only center in New York to perform TAE, regularly achieving significant shrinkage and reduction of the mass effect.
- The minimally invasive method, offered since 2023, can relieve respiratory and swallowing difficulties, with cosmetic improvements that enhance patients’ overall QOL.
- In addition to TAE, NYU Langone’s interventional thyroidology experts offer three other nonsurgical thyroid treatments: radiofrequency ablation, nanosecond pulsed field ablation, and ethanol ablation.
For decades, thyroid conditions such as goiters and nodules have been managed primarily through surgical resection. Beyond the risk of surgery-associated complications, patients often require lifelong thyroid hormone supplementation.
Over the past few years, leading centers such as NYU Langone Health’s Thyroid Program have helped develop interventional treatments that preserve healthy thyroid tissue and protect and maintain the gland’s function.
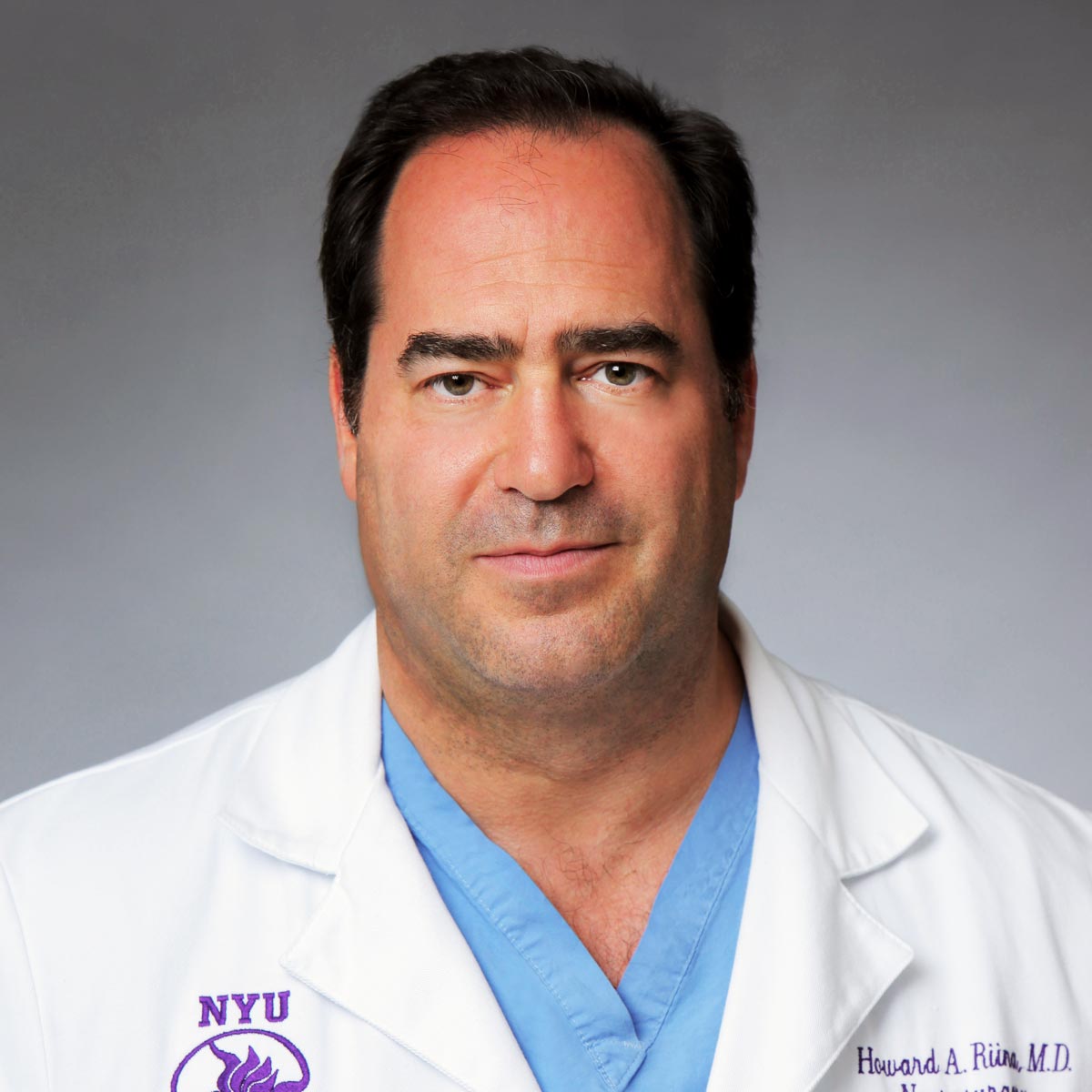
Thyroid artery embolization (TAE) is one such procedure. NYU Langone is one of the few centers in the country—and the only one in New York—to offer TAE, performed by neurosurgeon and embolization specialist Howard A. Riina, MD. To date, Dr. Riina has completed 15 TAE procedures, often achieving significant shrinkage and reduction of the mass effect.
“The reason I like particle embolization is I don’t close the vascular supply completely,” Dr. Riina says. “You could use glue, coils, or other things that permanently obstruct the vessels. But our goal is to shrink, so if we’re pruning the roots, so to speak, then the tumors will come down in size. But if we have to go back in and try again, we can do so multiple times if we use particle embolization.”
A Game-Changing Treatment for Large Goiters
In 2023, NYU Langone began offering TAE as a long-sought nonsurgical alternative for patients with abnormally enlarged thyroids, or goiters, that cause compression and extend into the chest. Kepal N. Patel, MD, chief of the Division of Endocrine Surgery and co-director of the Thyroid Program, says surgical removal of a large substernal goiter may require opening the chest. “For those patients, the thyroid artery embolization option has been very exciting, with impressive results,” Dr. Patel says. “This is what we call a game changer in the field.”
“This is what we call a game changer in the field.”
Kepal Patel, MD
“Some of the substernal goiters can be quite big,” Dr. Riina says. “They get wrapped around the great vessels and they displace the airway, often six or seven centimeters off midline, which is a lot.” As a result, patients can have both respiratory and swallowing difficulties.
After reviewing treatment options with patients, Dr. Patel refers appropriate candidates with symptomatic goiters to Dr. Riina. An angiogram helps map out each goiter’s blood supply. To treat them, Dr. Riina threads a long catheter through an artery in the patient’s wrist or groin and delivers millions of tiny polyvinyl alcohol particles to the inferior or superior thyroid artery or both.
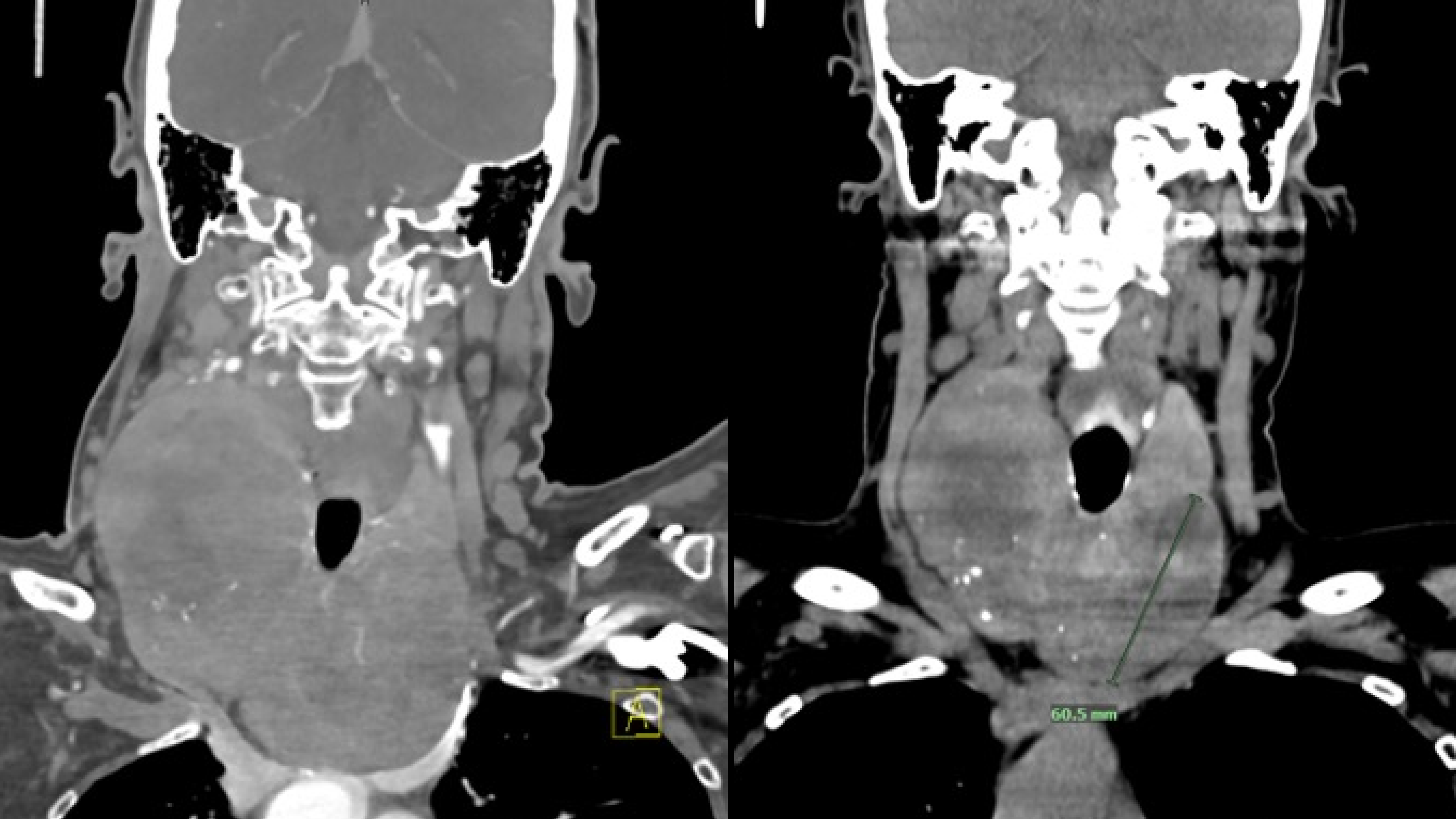
Through an ensuing restriction in blood supply to the gland’s dominant nodule, it gradually shrinks and relieves the compression, displacement, and other symptoms. To date, the procedure has yielded significant shrinkage in most cases, with the best results in lesions that remain highly vascular instead of fibrous.
Relieving Multiple Symptoms
For many of the patients, Dr. Riina says, the success can be seen through cosmetic changes to their neck and other quality of life improvements, like being able to wear a necklace or tight-collared shirt again. One patient took selfies to record the encouraging improvement to her neckline over time. Dr. Riina also successfully treated two brothers who had endured their goiters for years.
“One woman hadn’t been able to wear any jewelry for 30 years. She came back in for a follow-up appointment wearing a necklace, and she was ecstatic.”
Howard Riina, MD
“Yes, we want to address the disease and the airway compression and the swallowing. But for these patients, especially when it’s above the sternum, it’s disfiguring too,” Dr. Riina says. “One woman hadn’t been able to wear any jewelry for 30 years. She came back in for a follow-up appointment wearing a necklace, and she was ecstatic.”
Unexpectedly, the doctors have seen a bilateral effect in some cases in which embolization of only one side of the bow-tie-shaped gland yielded significant shrinkage of both sides. Dr. Riina suspects that bilateral shrinkage is due to particles that travel across the gland’s isthmus from one side to the other.
Excellence in Minimally Invasive Care
The colleagues are preparing a publication describing the TAE technique and results so far. Much of the success, Dr. Patel says, is due to Dr. Riina’s extensive expertise as a neuro-interventionalist. “For this procedure, you’re embolizing vessels in the neck: you’re going up the carotid, you’re embolizing the superior thyroid artery, the inferior thyroid artery,” Dr. Patel says. Embolizing those arteries can increase the risk of stroke and other complications, but Dr. Riina’s knowledge and experience has allowed him to achieve encouraging results while minimizing the risk.
Beyond TAE, the Thyroid Program’s interventional service offers three other minimally invasive treatments. One particularly welcome advance, Dr. Patel says, was the arrival of thyroid radiofrequency ablation (RFA), which uses thermal energy to destroy large noncancerous nodules. NYU Langone was one of the first medical centers in New York City to offer this treatment, in 2019. Another treatment, nanosecond pulsed field ablation, can also treat symptomatic thyroid nodules without thermal energy, making it potentially safer. Ethanol ablation can treat fluid-filled thyroid nodules, or cysts.