Referral Notes:
- RAGE406R, a novel small molecule inhibitor, blocks the interaction between RAGE and DIAPH1, a key driver of inflammation and tissue damage in diabetes.
- In mouse models, RAGE406R reduced inflammation and accelerated wound healing, and in primary macrophages, it dampened macrophage-driven immune responses.
- By targeting the intracellular signaling of RAGE rather than blood sugar, RAGE406R represents a promising new approach to treating complications of diabetes.
A study from NYU Langone Health published in Cell Chemical Biology identifies a novel small molecule inhibitor, RAGE406R, that prevents RAGE and DIAPH1 from interacting. The RAGE-DIAPH1 signaling axis is thought to be a major contributor of heart and kidney injury in diabetes, and slows the healing of related wounds.
When tested in mice, the experimental compound reduced inflammation and swelling in tissues affected by diabetes and drove faster tissue repair.
“There are currently no treatments that address the root causes of diabetic complications, and our work shows that RAGE406R can—not by lowering the high blood sugar, but instead by blocking the intracellular action of RAGE,” says co-senior study author Ann Marie Schmidt, MD, the Dr. Iven Young Professor of Endocrinology and a member of the Holman Division of Endocrinology, Diabetes, and Metabolism.
Improved Wound Healing
To explore its therapeutic potential, the team tested RAGE406R in a lead model of chronic diabetes complications: impaired wound healing in mice with obesity and type 2 diabetes. The data revealed that in both male and female diabetic mice, topical treatment with RAGE406R accelerated wound closure. In a model of delayed type hypersensitivity—the slower, T cell-mediated immune responses in diabetes that contribute to impaired wound healing—RAGE406R also reduced tissue swelling and erythema.
Macrophage-mediated inflammation is suggested to play a central role in impaired wound healing in diabetes. To test whether RAGE406R may be functioning as a macrophage antagonist, the researchers treated macrophages from patients with type 1 diabetes with RAGE406R and found reduced expression of CCL2 mRNA; CCL2 is a major chemokine used by macrophages to initiate inflammation.
“This key finding sets the stage for the expansion of experiments to test the effects of RAGE406R on multiple nodes in the inflammatory response,” the authors write.
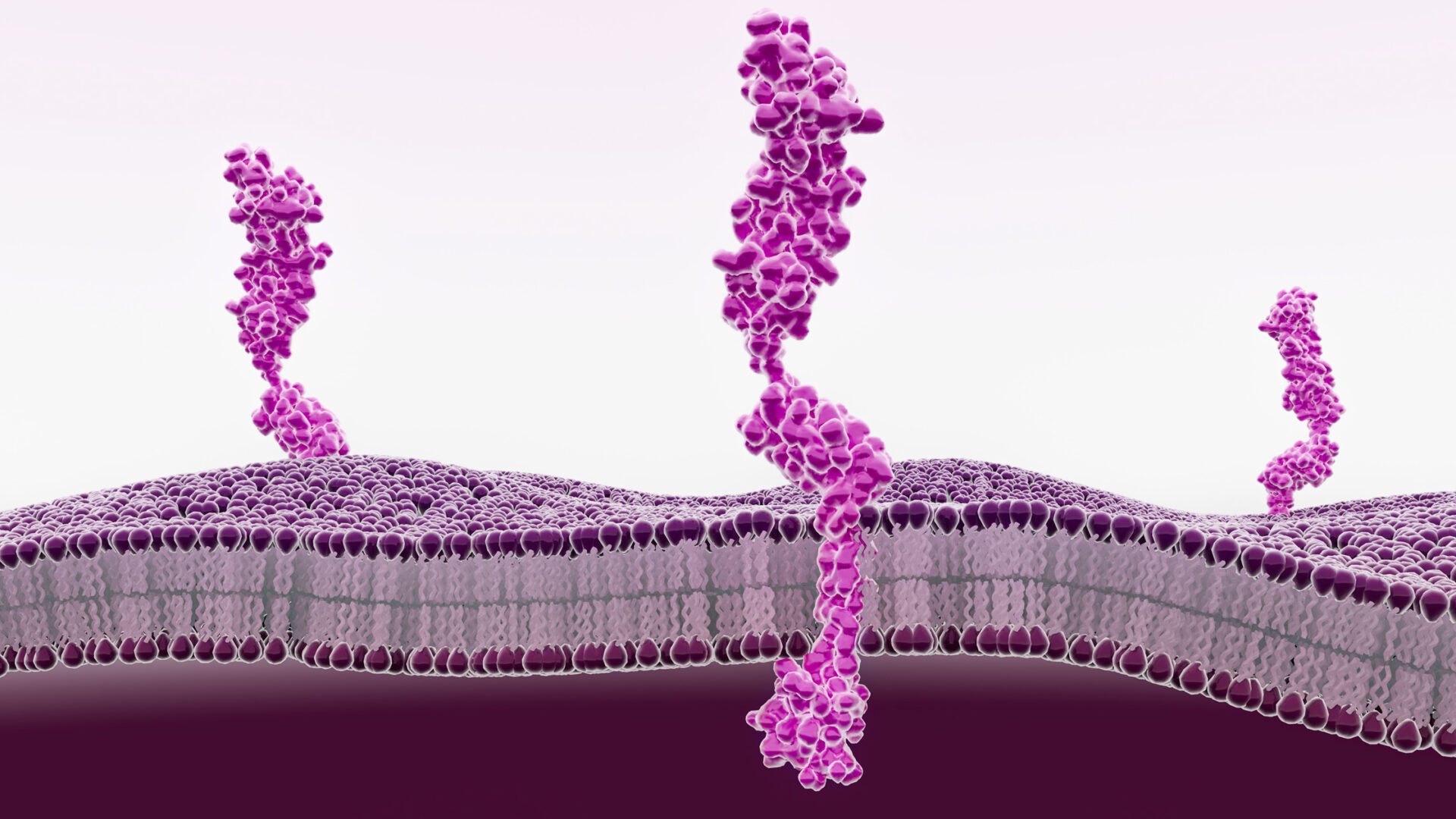
Mechanistic studies revealed that RAGE406R binds to the cytoplasmic tail of RAGE, blocking its interaction with DIAPH1, a regulator of the actin cytoskeleton. By preventing the formation of the RAGE-DIAPH1 complex, RAGE406R disrupts actin-mediated cellular changes that contribute to inflammation and tissue damage in diabetes.
Small Molecule Discovery
Previously, Dr. Schmidt’s team screened a library of more than 58,000 molecules and found a subset that competitively inhibited RAGE-DIAPH1 signaling. Their prior lead candidate, RAGE229, failed a standard test that detects if a compound has structure that may possibly change DNA code to create cancer risk. RAGE406R effectively eliminates the risk-creating part of RAGE229’s structure.
“If confirmed by future testing in human trials, the compound could potentially fill gaps in treatment by providing a disease-modifying therapeutic strategy for both types 1 and 2 diabetes.”
Disclosures
Dr. Schmidt is named as an inventor on patent applications owned by New York University that relate to the work detailed in the Cell Chemical Biology manuscript.