A new paper published in Alzheimer’s and Dementia finds that key biomarkers of neurodegeneration are elevated in patients hospitalized with COVID-19, potentially providing insight into the growing evidence of significant neurological effects in survivors of the illness. Some biomarkers matched or exceeded levels observed in patients with Alzheimer’s disease.
“Our study identified elevations of several blood-based markers specific to the central nervous system, including neuronal and glial markers,” says Jennifer A. Frontera, MD, who led the NYU Langone Health research team and is a member of the World Health Organization’s Brain Health Neurology and COVID-19 Forum.
“The finding that markers of neurodegeneration are high in patients with severe COVID-19—who have no prior history of cognitive decline—adds support to the idea that the extended states of hypoxia and hyperinflammation in these patients may be having a significant impact on brain function,” says study co-author Thomas M. Wisniewski, MD, director of the Center for Cognitive Neurology and the Pearl I. Barlow Center for Memory Evaluation and Treatment.
“The finding that markers of neurodegeneration are high in patients with severe COVID-19—who have no prior history of cognitive decline—adds support to the idea that the extended states of hypoxia and hyperinflammation in these patients may be having a significant impact on brain function.”
Thomas M. Wisniewski, MD
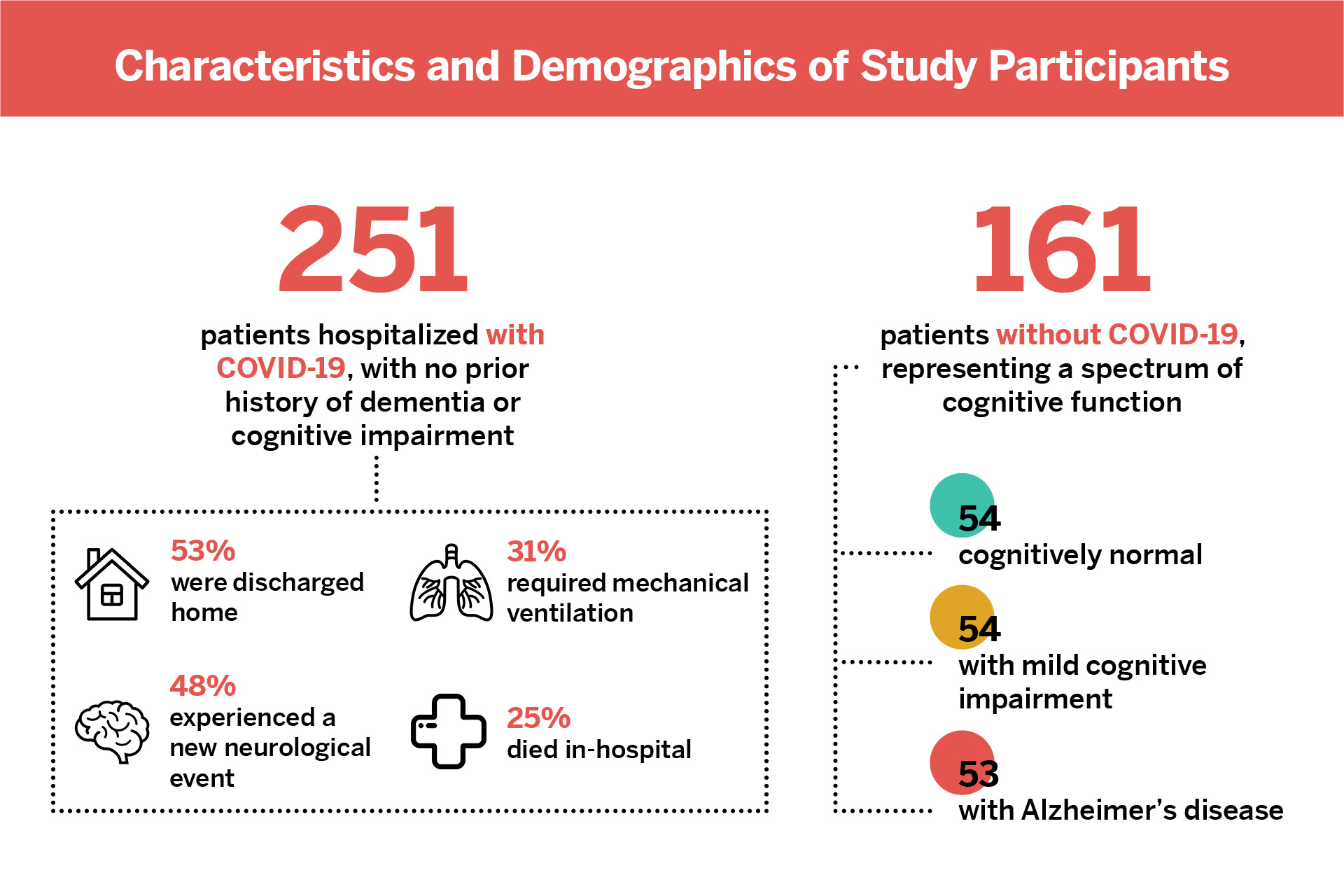
Of the 251 patients with COVID-19 included in the study, 48 percent had new neurological events occur during hospitalization, with toxic-metabolic encephalopathy being the most common diagnosis.
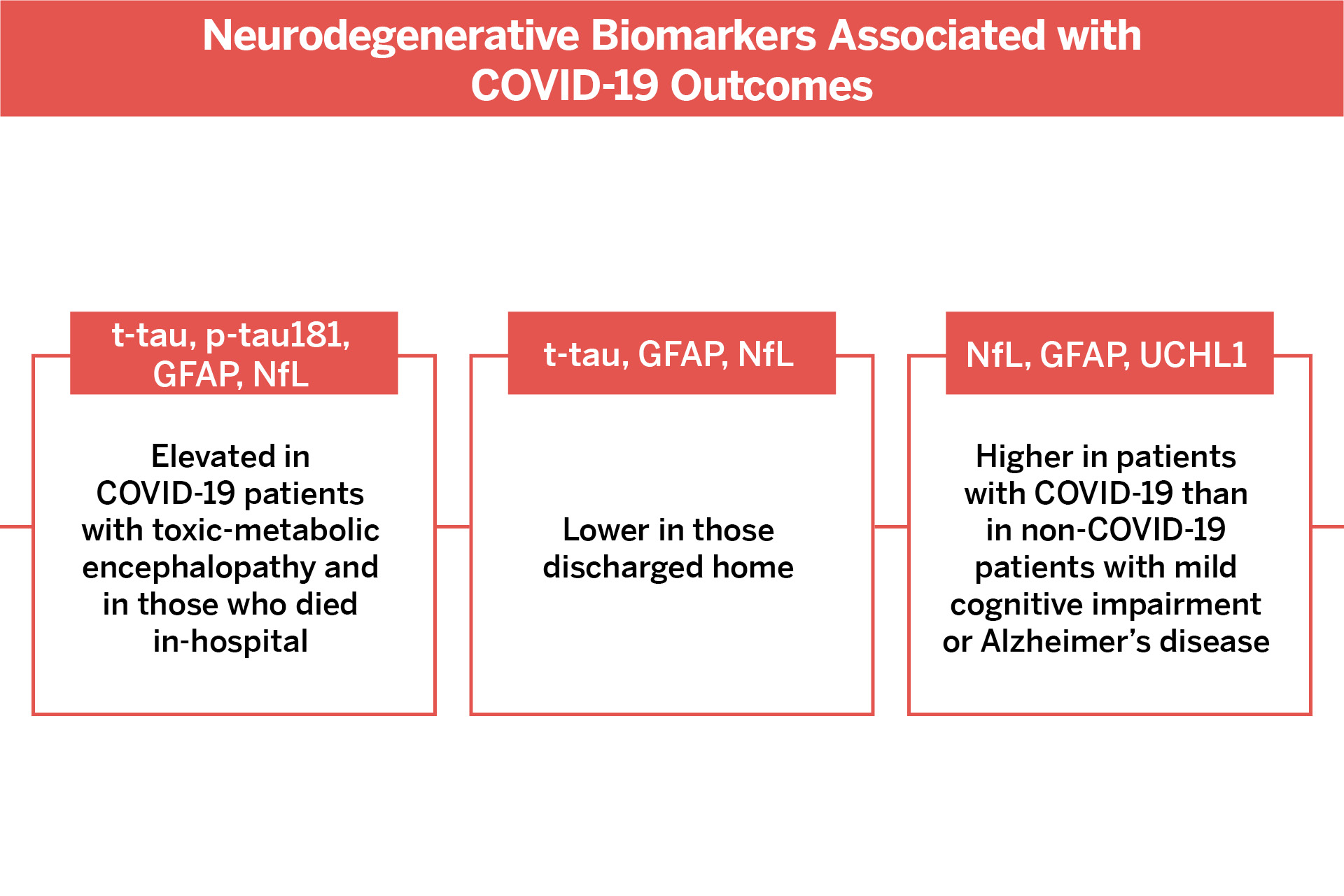
Overall, the neurodegenerative biomarkers found to correlate most strongly with COVID-19 severity and risk of encephalopathy were total tau (t-tau), phosphorylated tau-181 (p-tau181), glial fibrillary acidic protein (GFAP), and neurofilament light chain (NfL).
Strikingly, levels of three biomarkers—GFAP, NfL, and ubiquitin carboxy-terminal hydrolase 1 (UCHL1)—were as high or even higher in patients hospitalized with COVID-19 than in non-COVID patients with Alzheimer’s disease.
“More research is needed to track the trajectories of these biomarkers and their associations with poor cognitive outcomes in survivors of COVID-19,” says Dr. Frontera.
“More research is needed to track the trajectories of these biomarkers and their associations with poor cognitive outcomes.”
Jennifer A. Frontera, MD