Collaborative Evaluation Helps Diagnose and Relieve Pudendal Neuralgia
A woman in her early 40s presented to NYU Langone Health for an evaluation of stress urinary incontinence and vaginal pain that had persisted since her second vaginal delivery four years prior. Although that delivery was uncomplicated, it required an episiotomy and the woman began experiencing constant irritation and burning in her vaginal opening and sometimes in her rectum.
“Pudendal neuralgia falls through the cracks because patients are not knowledgeable about it and most healthcare providers have never heard of it.”
Nirit Rosenblum, MD
Through a careful and thorough evaluation, urologist Nirit Rosenblum, MD, and pain specialist Meera K. Kirpekar, MD, developed high suspicion of a neuropathic condition called pudendal neuralgia. “I think pudendal neuralgia falls through the cracks because patients are not knowledgeable about it and most healthcare providers have never heard of it,” Dr. Rosenblum says.
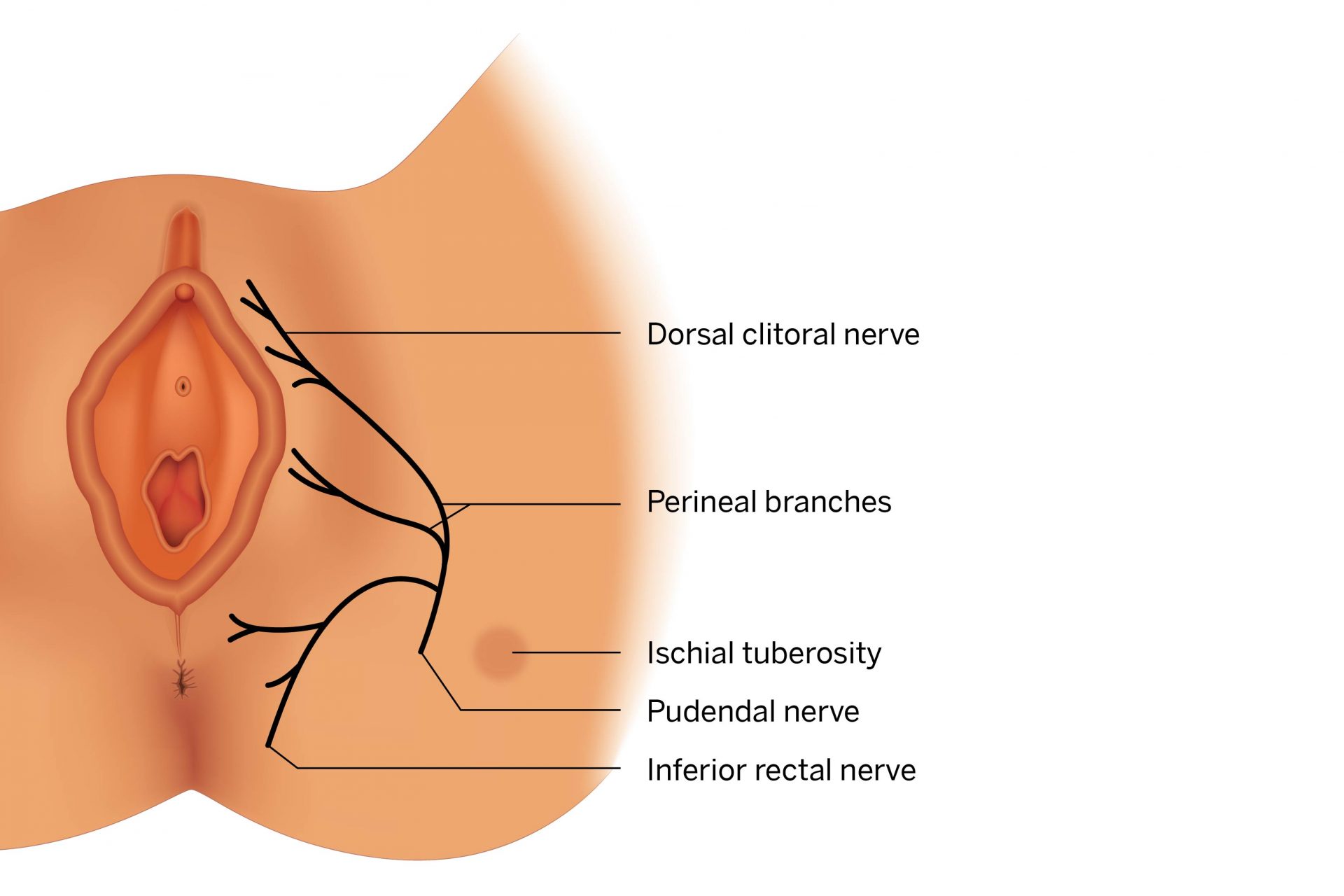
The pudendal nerve originates at the base of the spine and descends through the gluteal muscles until it reaches the pelvic floor, where it splits into three major branches. Damage to the nerve can cause overactive bladder syndrome and mimic a host of other conditions.
“If you block the pudendal nerve and there is at least 50 percent pain relief lasting the duration of the local anesthetic, you have diagnosed pudendal neuralgia.”
Meera K. Kirpekar, MD
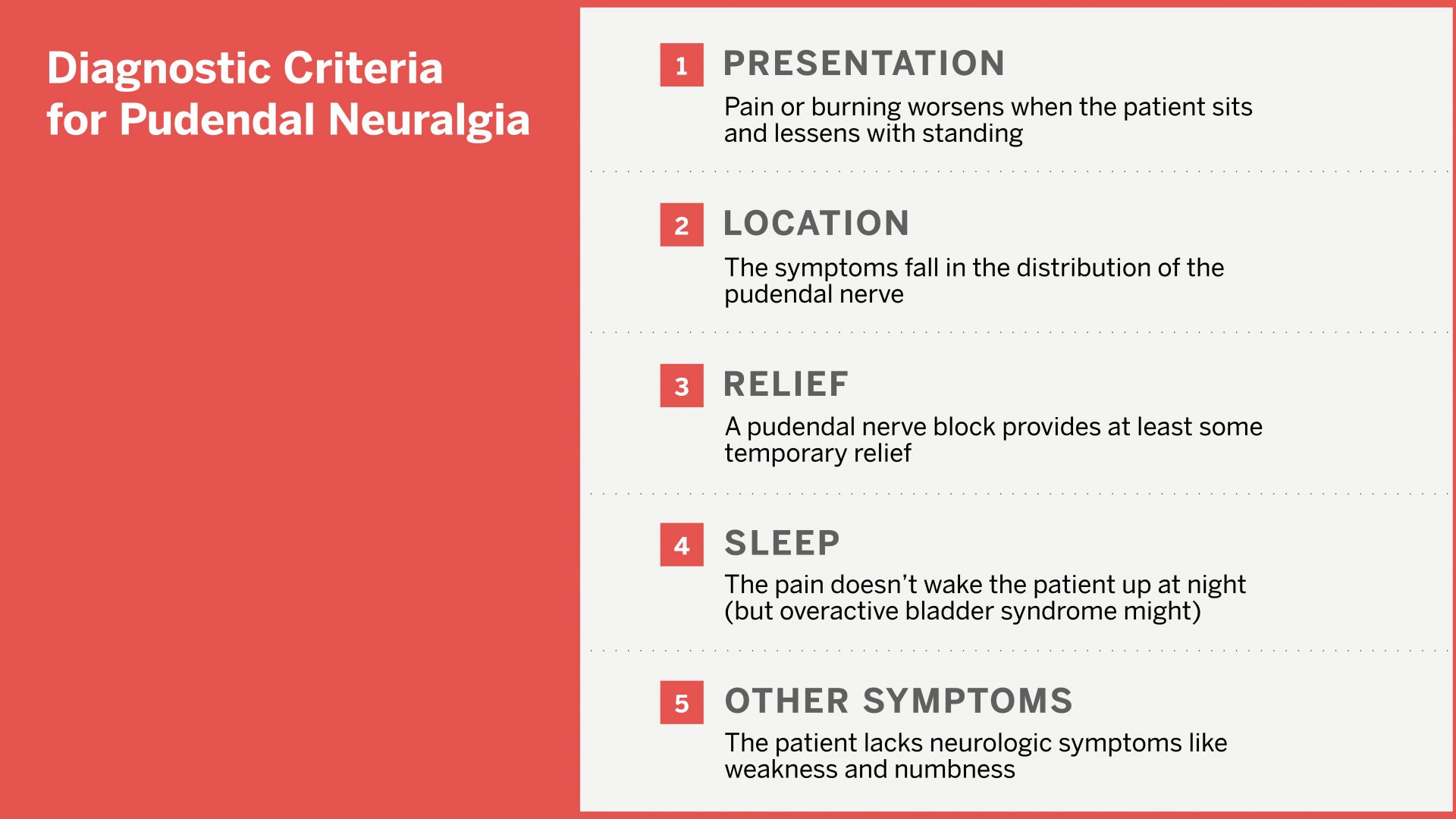
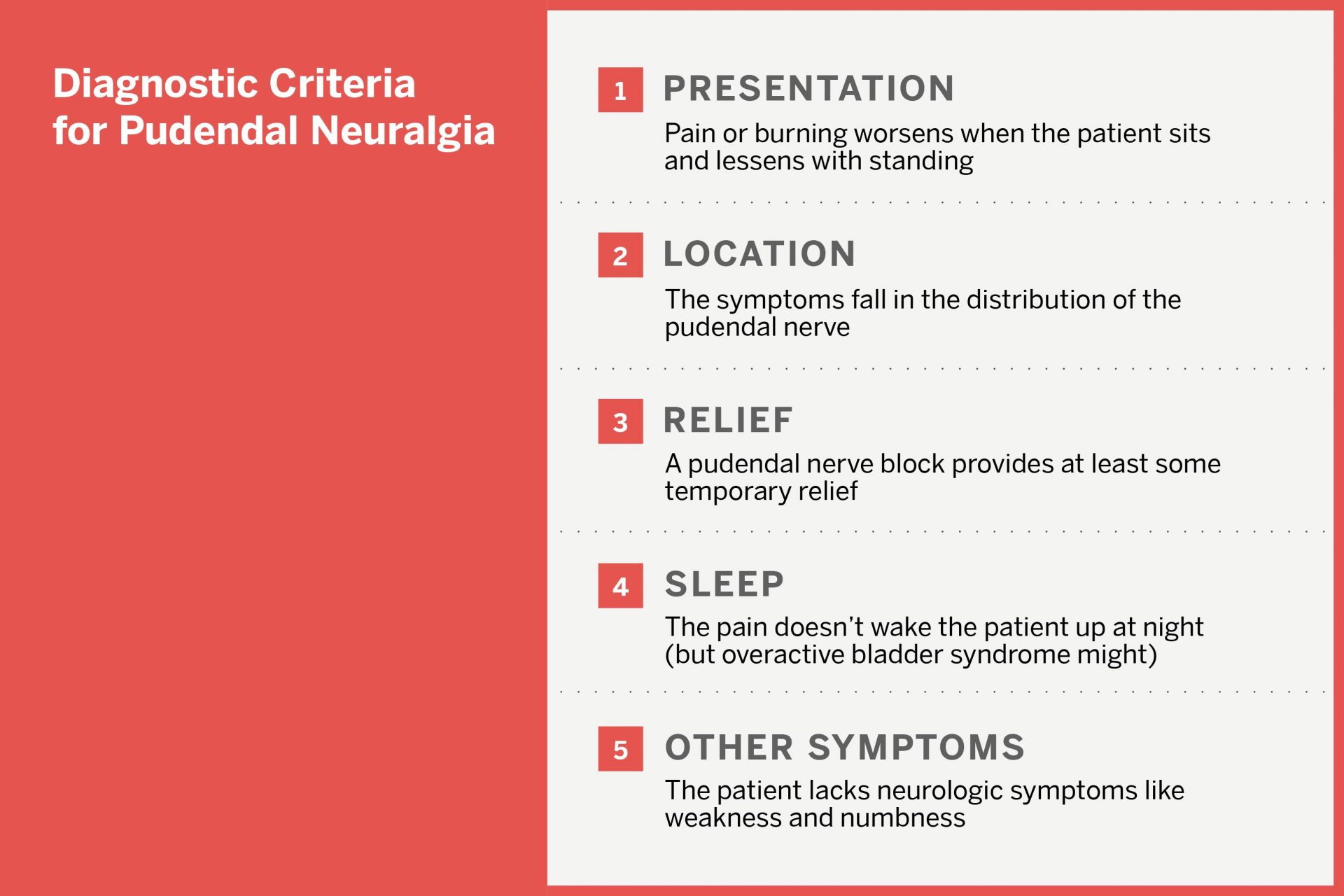
One telling clue was a burning sensation in the patient’s vaginal introitus that intensified when she sat for long periods or sat on a hard surface. Pain that worsens with sitting but lessens with standing is consistent with compression of the pudendal nerve along its pathway across the ischial tuberosity.
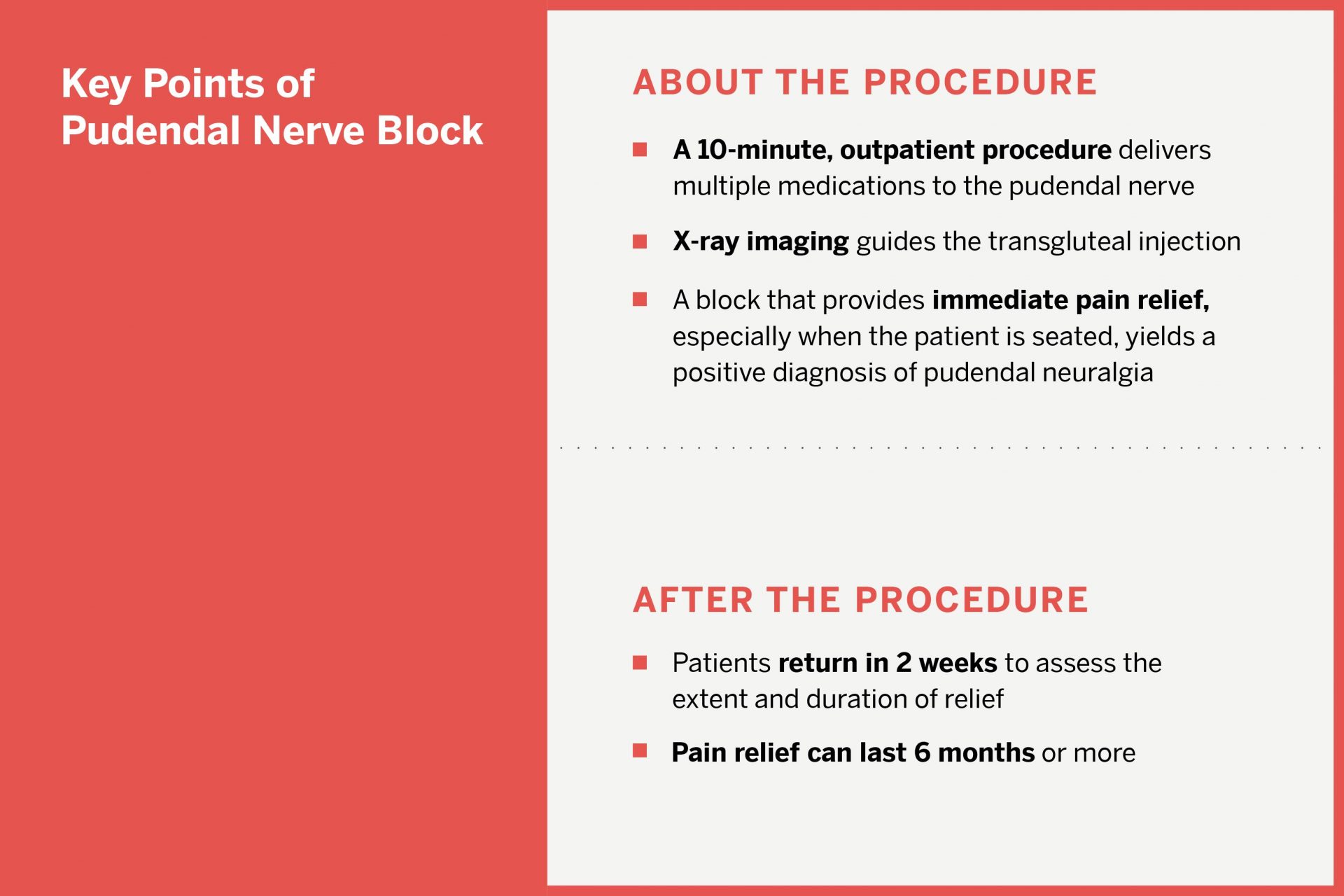
Dr. Kirpekar performed a pudendal nerve block, which can be both therapeutic and diagnostic. “If you block the pudendal nerve and there is at least 50 percent pain relief lasting the duration of the local anesthetic, you have diagnosed pudendal neuralgia,” she says.
After the 10-minute, X-ray-guided injection, the patient achieved full pain relief. “She was thrilled,” Dr. Kirpekar says. By four months, some slight pain had returned, but it was not interfering with the woman’s daily activities, and the physicians are continuing to monitor her progress.