To improve the quality and efficacy of colonoscopy, reduce polyp miss rates, and optimize adenoma detection rates, endoscopists at NYU Langone Health are working with computer-aided polyp detection (CADe) systems that act as a second set of eyes.
National, multicenter clinical trials evaluating artificial intelligence (AI) in colonoscopy have solidified the technology’s role as a true aid, with NYU Langone researchers Seth A. Gross, MD, and Aasma Shaukat, MD, MPH, involved in two such studies.
“Our findings add to the growing amount of literature that shows using computer-aided technology during an endoscopy procedure can improve the quality of exams performed and improve outcomes for our patients,” says Dr. Shaukat, epidemiologist and director of outcomes research for the Division of Gastroenterology and Hepatology.
“Our findings add to the growing amount of literature that shows using computer-aided technology during an endoscopy procedure can improve the quality of exams performed and improve outcomes for our patients.”
Aasma Shaukat, MD, MPH
“As the role of artificial intelligence in endoscopy grows, we are making sure that it is adding value to patient care,” says Dr. Gross, advanced endoscopist and clinical chief of the Division of Gastroenterology and Hepatology.
AI as a Proven Aid
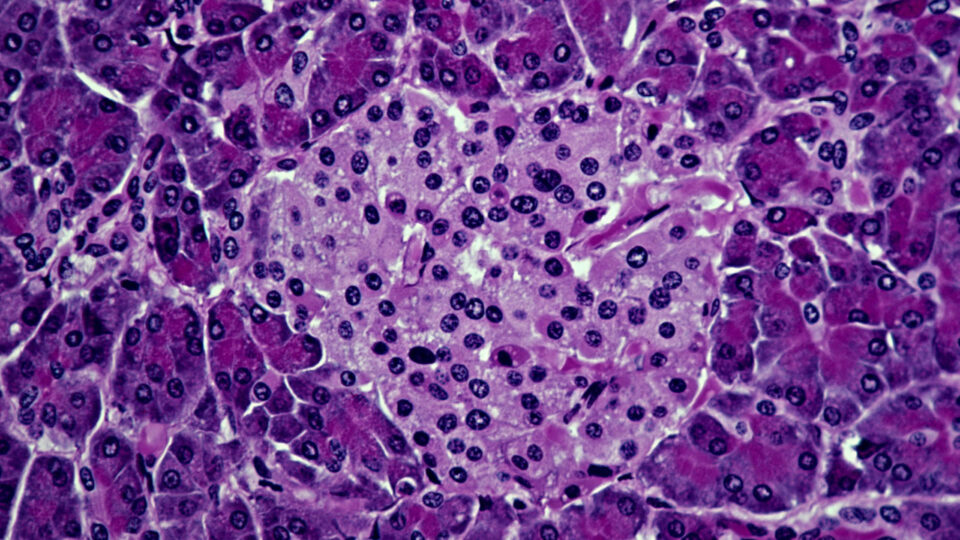
Reported in Gastroenterology, Dr. Shaukat led a large randomized controlled trial that evaluated a CADe device, SKOUT, in colonoscopy procedures. Involving nearly 1,500 participants, the study found the device increased the adenomas per colonoscopy (APC) rate by 27 percent, from 0.83 to 1.05, while causing no increase in resection of non-neoplastic lesions.
Notably, the device supported a 20 percent increase in the detection of small (1 to 4 millimeter) lesions and a 29 percent increase in the detection of larger (5 to 9 millimeter) lesions, challenging a criticism that AI systems only increase the detection of diminutive polyps.
“Use of the CADe system enabled an increase in the detection of large lesions particularly in the proximal colon, which is of great interest as studies suggest traditional colonoscopy is not as effective at preventing proximal cancers,” Dr. Shaukat says.
Dr. Shaukat has also published her findings on AI-assisted colonoscopy improving detection of polyps for endoscopists with all experience levels, and without increasing removal of polyps with normal histology.
Building on Early Success
The trial builds on one of the first randomized controlled trials of CADe for screening and surveillance colonoscopy in the United States. Published in Clinical Gastroenterology and Hepatology with Dr. Gross as a co-author, that study found an increase in APC and a decrease in the miss rate of adenomas, polyps, and sessile serrated lesions with the use of the CADe device EndoScreener.
“When you find large adenomas and sessile serrated lesions, those are always value-add. But we’re coming to a period where the question can be raised, ‘What’s the long-term benefit when you find a very small adenoma? How does it impact the patient’s life?’” Dr. Gross says. “We’ll probably never know that information because when we see a polyp, we remove it.”
“We’re coming to a period where the question can be raised, ‘What’s the long-term benefit when you find a very small adenoma? How does it impact the patient’s life?’”
Seth A. Gross, MD
Both EndoScreener and SKOUT have received 510(k) clearance from the U.S. Food and Drug Administration (FDA) for colorectal cancer screening and surveillance.
Rethinking Surveillance Given New Demands
An increase in polyp detection rates with the use of AI also means an increase in the number of patients requiring surveillance. Yet, this is another area in which AI may provide solutions, says Dr. Gross, by better risk-stratifying patients based on what is found during colonoscopy.
Updates to colorectal cancer surveillance guidelines from the U.S. Multi-Society Task Force, of which Drs. Shaukat and Gross are members, are also serving to address this concern.
“For very small precancerous polyps, what used to be a five-year interval is now a seven-year interval, what used to be a guaranteed three-year interval is a three- to five-year interval,” Dr. Gross says.
“These adjustments are made based on studies and outcomes data. You don’t want to bring someone back for a very diminutive, precancerous polyp when they could probably wait a little bit longer. Hopefully that will balance out what the technology does in terms of identifying more patients to follow.”
Disclosures
Dr. Gross has served as a consultant for Olympus and Medtronic. Dr. Shaukat reports research funding to NYU Langone Health for the current manuscript from Iterative Scopes and consulting fees from Freenome Inc.