By detailing the essential roles of metabolic enzymes in bladder cancer, researchers at NYU Langone Health and Perlmutter Cancer Center have identified novel therapeutic strategies that may help in overcoming cisplatin resistance. The innovative approaches take aim at two glycolytic enzymes—enolase-1 and PKM2—shown to promote tumor growth by enhancing the functions of oncogenes.
“In almost every bladder tumor type, we find both of these enzymes are over-expressed,” says Xue-Ru Wu, MD, principal investigator of the research team and the Bruce and Cynthia Sherman Professor of Urological Research and Innovation.
Preliminary data also indicate both enzymes are induced by cisplatin, suggesting a role in acquired resistance. “If we take cells grown in culture, expose them to increasing concentrations of cisplatin, and then look at these enzymes, they’re markedly induced,” says Dr. Wu.
“We show that the two enzymes play different roles. Enolase-1 can drive tumor initiation while PKM2 supports tumor promotion.”
Xue-Ru Wu, MD
Efforts are now underway to identify and test inhibitors that can be used in combination with cisplatin and other chemotherapies.
Metabolism and Malignancy
Reprogrammed metabolism is a hallmark of cancer. While healthy cells rely heavily on oxidative phosphorylation, cancer cells commonly switch to aerobic glycolysis to fuel their uncontrolled growth.
Yet, “bladder cancer metabolism is an area that people have paid relatively little attention to,” says Dr. Wu.
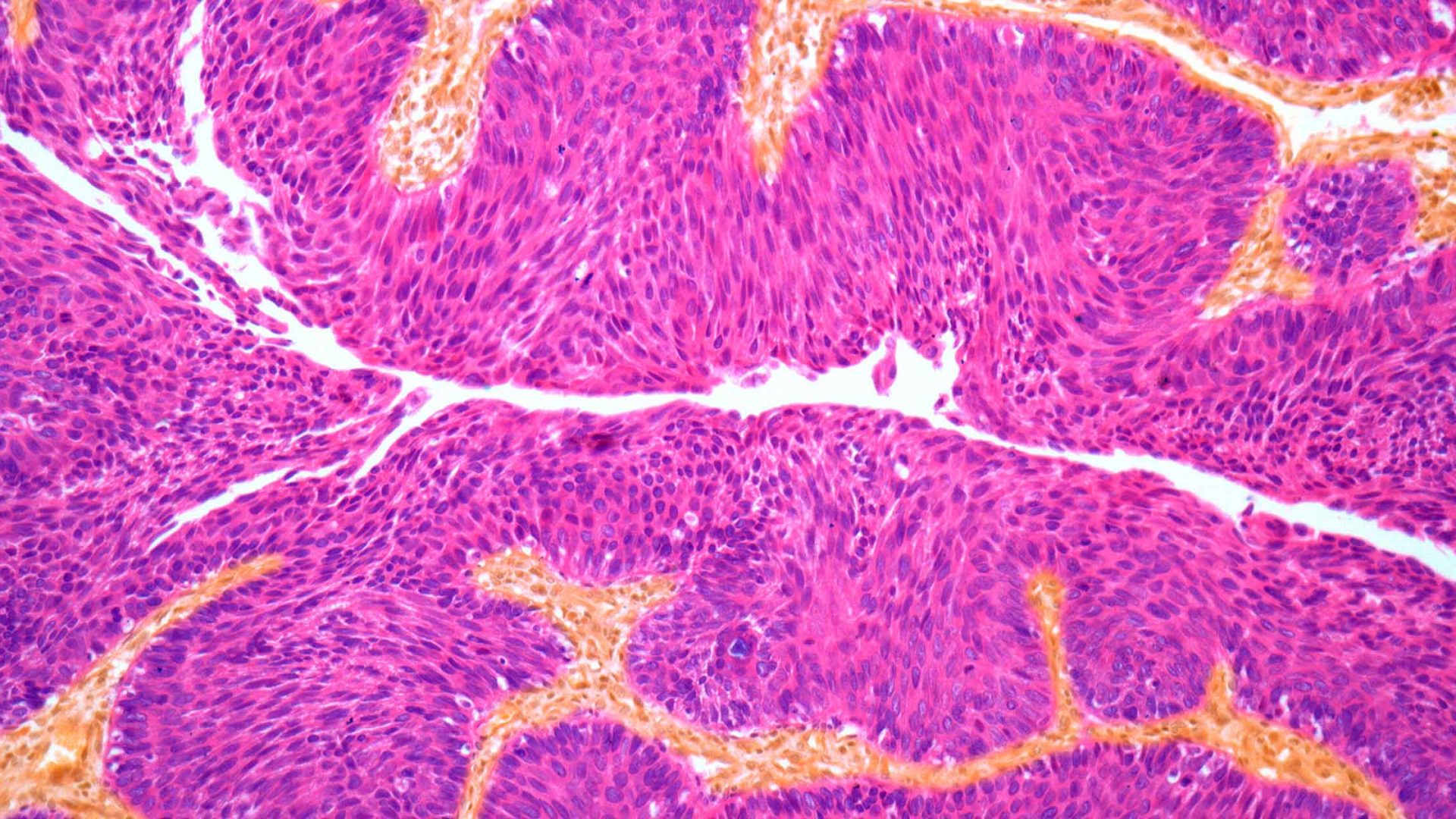
In studying the process, his team discovered that some glycolytic enzymes not only prop up the proliferative metabolism of bladder cancer cells but also moonlight as oncogenes by tempering the normal function of tumor suppressors.
This was demonstrated in a 2021 report from his group in Nature Communications, which revealed that enolase-1, a main glycolytic enzyme, functionally disables CDK inhibitors 4 and 6, leaving cell cycle progression unchecked. A subsequent study from the group in Cancer Research reported that PKM2, another key glycolytic enzyme, enhances angiogenesis by augmenting the angiogenic factor STAT3.
“We show that the two enzymes play different roles,” says Dr. Wu. “Enolase-1 can drive tumor initiation while PKM2 supports tumor promotion.”
Overcoming Cisplatin Resistance
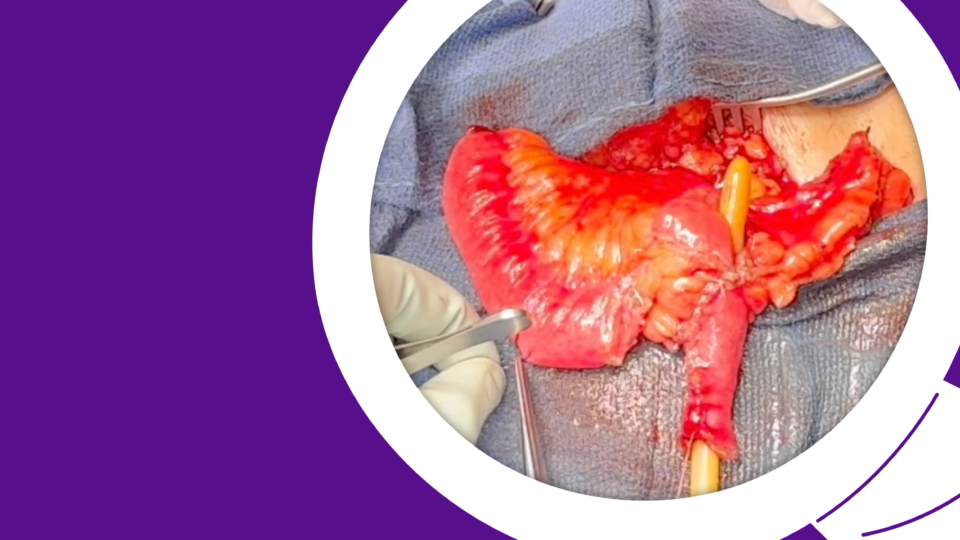
The next step is to identify inhibitors of the enzymes, which Dr. Wu and colleagues are pursuing by repurposing existing drugs and by screening for new agents.
Pairing these inhibitors with cisplatin-based chemotherapies may serve to address resistance and improve treatment efficacy, all while minimizing treatment-associated toxicities. According to Dr. Wu, similar ideas are being tested in other cancer types, but little focus has been placed on bladder cancer.
“Utilizing the tumor cell’s metabolic bypass to overcome chemotherapy-based treatment resistance is very attractive. It’s preferable that you target a pathway that’s different from those targeted by existing therapeutics, and this approach does just that.”
“Utilizing the tumor cell’s metabolic bypass to overcome chemotherapy-based treatment resistance is very attractive,” says Dr. Wu. While it’s common to address resistance by increasing the dosage of the chemotherapy being used or by pairing it with a second chemotherapy, he stresses this usually comes with increased toxicity.
“It’s preferable that you target a pathway that’s different from those targeted by existing therapeutics, and this approach does just that.”
NIH and VA Support
Funding for the work comes from a multimillion-dollar NIH Program Project (P01) grant supporting innovative bladder cancer research in the laboratories of Dr. Wu and colleagues Diane M. Simeone, MD, and Moon-Shong Tang, PhD. Initially awarded in 2013, the grant is in its second funding cycle.
“The key focus of this grant is to look at how the different bladder cancer subtypes arise and progress to inform biomarkers and therapeutics,” says Dr. Wu.
Dr. Wu’s research has also been funded by the VA Health Services Research and Development Service.
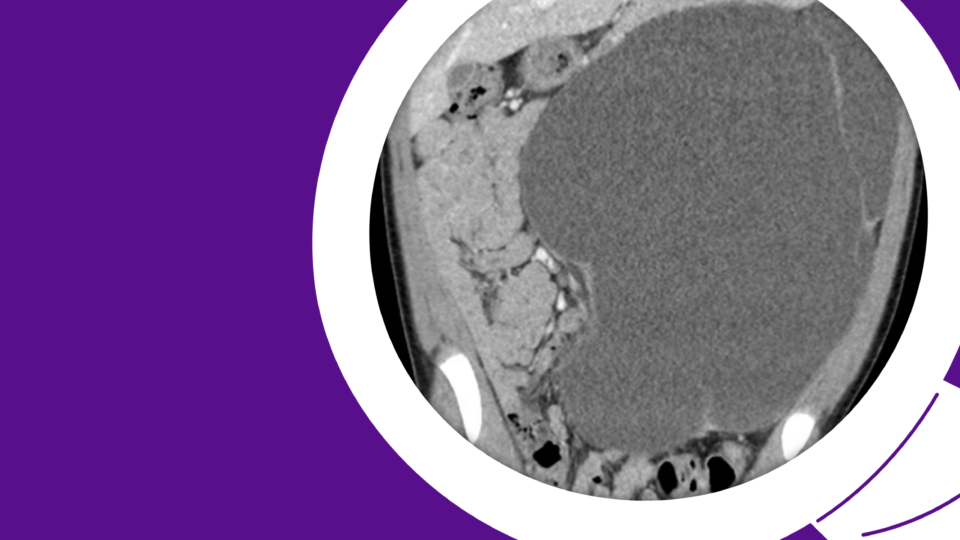
“In 2023, it’s estimated that 82,000 new cases of bladder cancer will be diagnosed,” he adds. “It’s a lifelong disease, it’s highly recurrent, and it’s extremely under-studied. While we have immunotherapy, only about 25 percent of patients respond. For the remaining 75 percent of patients with muscle-invasive disease that doesn’t respond, we need to treat them differently.”