Referral Notes:
- NYU Langone researchers have identified a low-cost, immediately actionable strategy to reduce instability and hip dislocation following THA.
- Their study evaluated more than 8,600 fixed-bearing THAs, identifying a dramatic 86 percent reduction in dislocation risk when the largest possible femoral head size was used.
- The benefit persisted across surgical approaches, implant systems, robotic versus manual techniques, and body types.
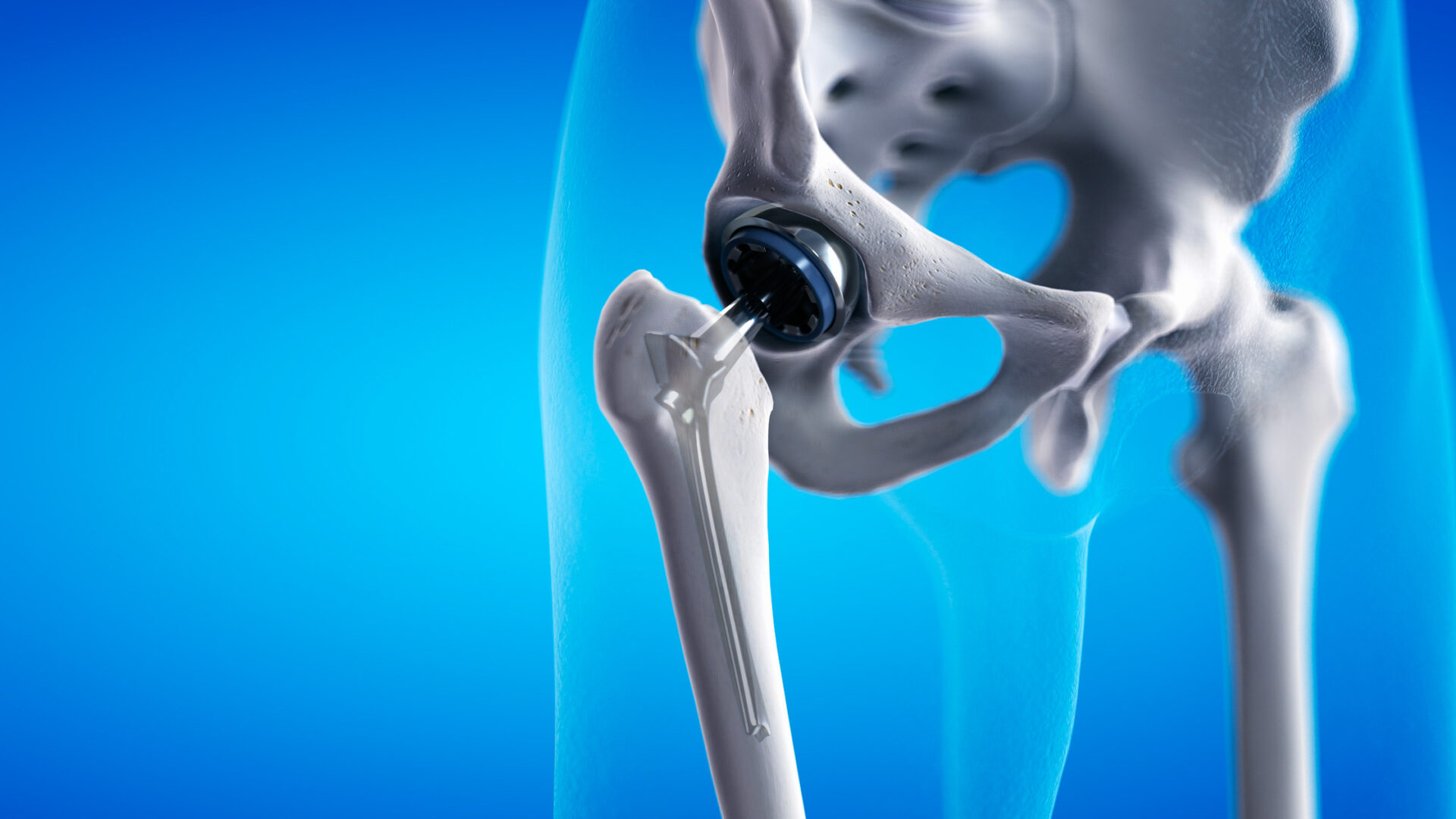
A simple, low-cost operative choice—selecting the largest possible femoral head size—can significantly reduce the risk of dislocation after fixed-bearing total hip arthroplasty (THA), according to an NYU Langone Orthopedics study presented at the 2025 American Association of Hip and Knee Surgeons Annual Meeting.
The findings suggest a straightforward answer to an ongoing question facing surgeons: how to reduce the risk of instability and dislocation after THA, and thereby decrease patient morbidity and revision burden.
“Surgeons may have hesitated to use the largest available bearing diameter. This data suggests we should be more deliberate in choosing the largest safe option.”
Matthew Hepinstall, MD
“Surgeons may have hesitated to use the largest available bearing diameter out of desire for a thicker polyethylene liner and doubt that the largest bearing would substantially improve stability,” says lead author and orthopedic surgeon Matthew Hepinstall, MD. “But this data suggests we should be more deliberate in choosing the largest safe option.”
Head Size and Stability
In a retrospective review of 8,607 patients who underwent primary fixed-bearing THA—about 10 percent of whom received the maximum femoral head size allowable for their anatomy—researchers found clear evidence supporting the larger bearings:
- Zero dislocations occurred among the 835 patients who received maximized bearings.
- 79 dislocations occurred in the non-maximized cohort, for which 7,309 received the second-largest bearing available and 463 received smaller bearings.
- Even after accounting for surgical approach, robotic use, or patient body type, use of the largest-possible bearing diameter reduced the odds of dislocation by 86 percent.
Notably, robotic surgery also reduced dislocation rates by 65 percent, computer-navigated procedures by 10 percent, and lateral and anterior approaches by 52 and 38 percent, respectively, but maximizing bearing size had the largest protective effect.
“Maximizing head size offers even greater protection against dislocation than some of the most sophisticated surgical tools.”
“We found that maximizing head size offers even greater protection against dislocation than some of the most sophisticated surgical tools at our disposal,” notes Dr. Hepinstall. “This benefit held across approaches and implant systems, supporting maximizing diameter as a baseline safeguard against instability.”
Challenging the Status Quo in Implant Selection
This large-scale analysis, one of the first to isolate bearing maximization as a variable across multiple implant systems, offers a simple intraoperative strategy to improve outcomes—particularly valuable as case complexity and surgical volumes increase.
The authors note that longer-term studies will be valuable to assess polyethylene wear or liner edge-loading over time, particularly in high-demand patients. However, registry data suggests that modern cross-linked polyethylene tolerates large heads well, making this a low-risk adjustment in most cases.
“Maximizing bearing size is low cost, technically straightforward, and immediately actionable,” adds Dr. Hepinstall. “It’s a practical step surgeons can take—without new implants or instruments—to deliver safer, more reliable results.”