Resolving a Complex Cascade of Symptoms
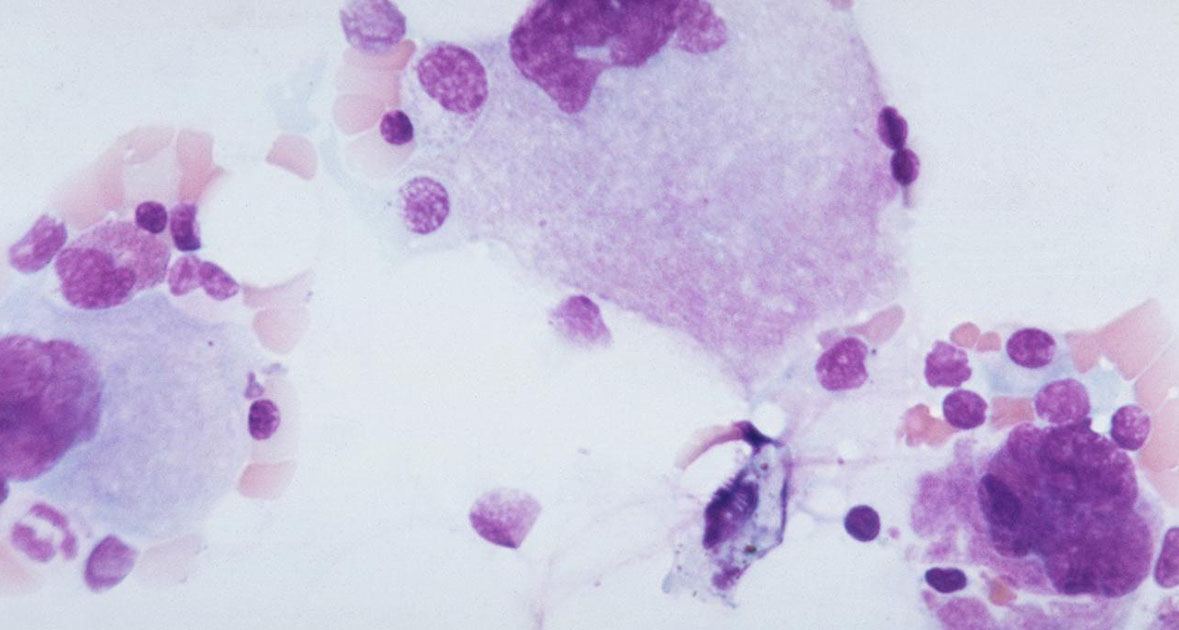
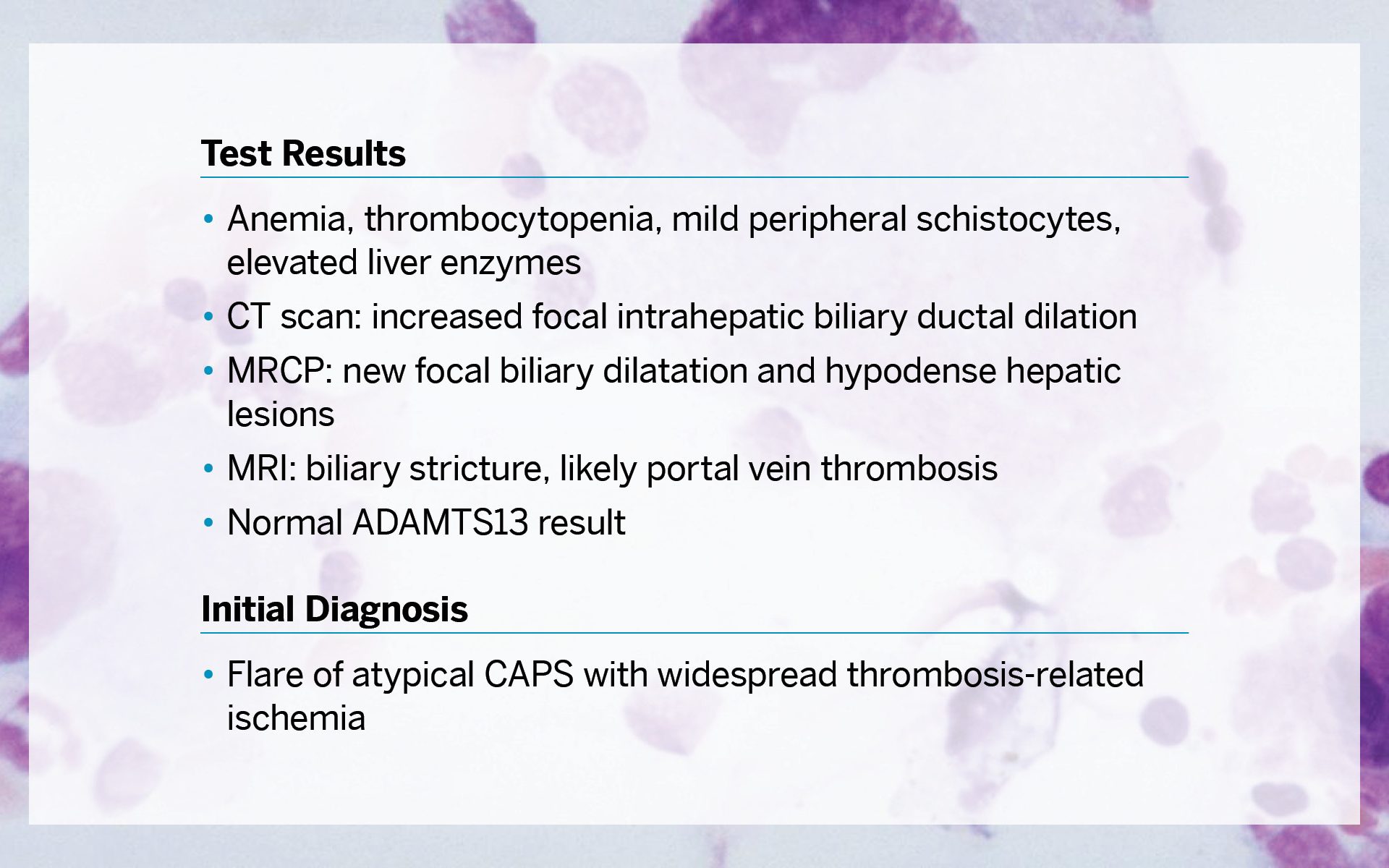
A 35-year-old female was admitted via the ED at NYU Langone Health’s Tisch Hospital with one week of fever, nausea, intense abdominal pain, and diffuse bone pain. She had a history of systemic lupus erythematosus (SLE), secondary antiphospholipid syndrome (APS) with a triple-positive aPL antibody profile, HELLP syndrome, and chronic thrombocytopenia.
Given the patient’s medical history, lab and imaging results, fever, and intense pain, H. Michael Belmont, MD, co-director of the Lupus Center, concluded that her presentation reflected a flare of atypical catastrophic APS (CAPS) with widespread thrombosis-related ischemia with involvement in her bone, bone marrow, and hepatobiliary tract.
“This patient was highly complex, with her lupus and secondary antiphspholipid syndrome unmasking an underlying genetic defect that also gave her complement-mediated HUS.”
H. Michael Belmont, MD
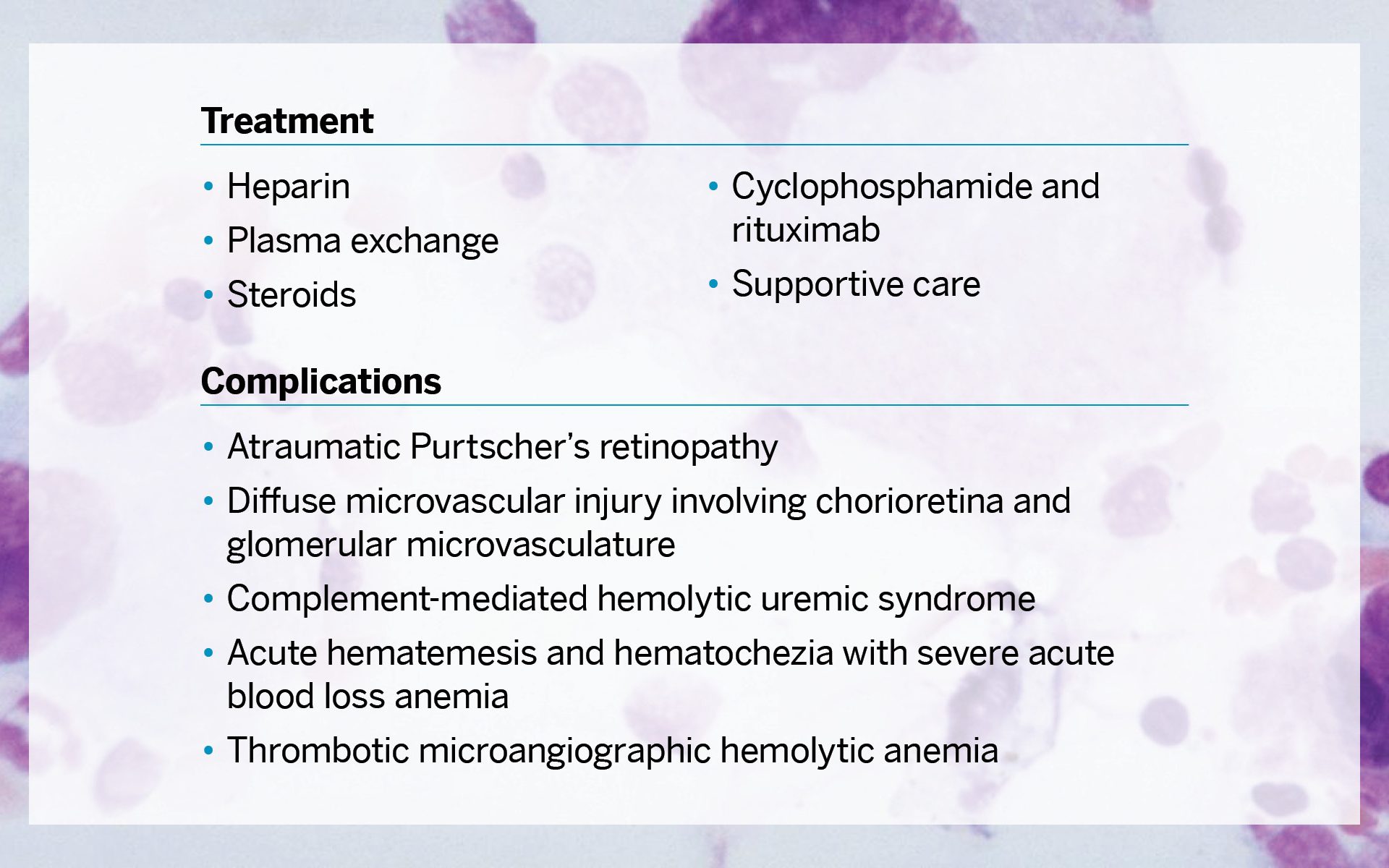
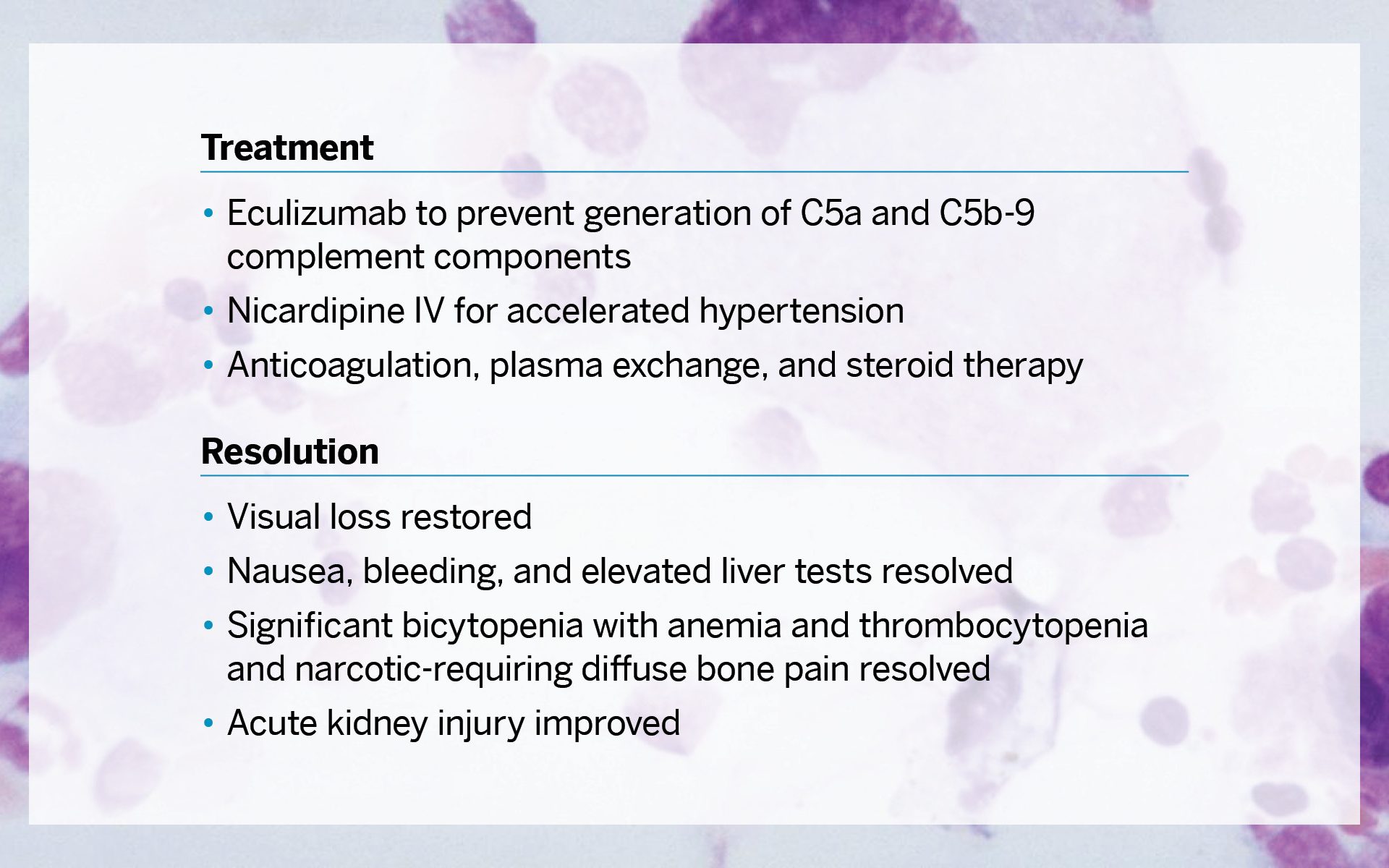
Worsening symptoms, including acute bilateral blurry vision and a nonoliguric acute kidney injury with nephrotic range proteinuria, led Dr. Belmont and colleagues to order atypical hemolytic uremic syndrome (aHUS) genetic testing. The test revealed variants in both the CFB and MCP (CD46) genes for complement regulatory proteins.
“This patient was highly complex, with her lupus and secondary antiphospholipid syndrome unmasking an underlying genetic defect that also gave her complement-mediated HUS,” he says.
Effectively managing and eventually resolving the case relied on unveiling and treating the atypical HUS and consulting with specialists in multiple departments to address the refractory CAPS complicated by bone, bone marrow, liver, biliary, choroid/retina, kidney, and jejunum involvement.
One month after her hospital admission, the patient was well enough to be discharged. “Close and frequent consultations allowed our interdisciplinary care team to quickly respond to an evolving and cascading suite of symptoms,” says Dr. Belmont.