Referral Notes:
- Patients with hip fractures have better postsurgical outcomes, with fewer complications, when discharged to home instead of a rehabilitation center.
- A new NYU Langone Orthopedics study finds that reinforcing “home is best” messaging can yield a significant increase in discharge to home rates, from 33.1 to 47.5 percent.
- The study found that nursing and physical therapy staff and patient care technicians were key to the quality initiative’s success, given their frequent interactions with patients.
Multiple studies have found that patients with hip fractures fare better after surgery when they can recover at home. Nonetheless, orthopedic surgeon Nicole M. Stevens, MD, often finds herself correcting the misconception that patients recover faster in a rehabilitation center.
Through a recent “home run” awareness campaign, Dr. Stevens and colleagues significantly improved the discharge to home rate for patients undergoing surgery for hip fractures without increasing the rate of total readmissions. “The purpose of our initiative was to create cohesive messaging for all hospital personnel that interact with hip fracture patients, to really drive home this message that home is the best place for a patient to be,” she says. “If they can safely go home, that is better for them.” The study was recently submitted for publication.
“Home is the best place for a patient to be. If they can safely go home, that is better for them.”
Nicole M. Stevens, MD
As a vehicle for that messaging, her team created a badge buddy consisting of a tag filled with key information and talking points. The researchers gave the tag to all members of the hip fracture care team to wear with their ID badges so that the information would be readily available when talking to patients and their families.
No Place Like Home
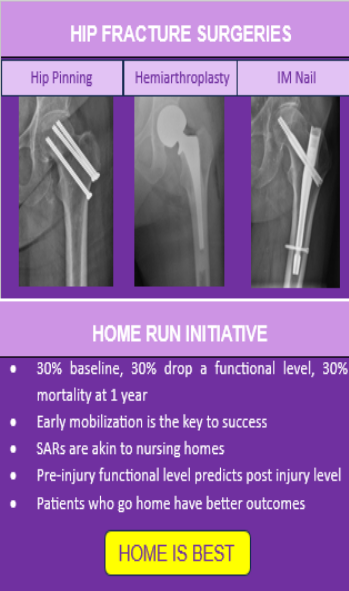
The tag’s front depicts the three main kinds of hip fracture surgery—hip pinning, hemiarthroplasty, and intramedullary (IM) nail—to show patients what their procedure will look like. The tag’s back includes talking points for staff, such as emphasizing early mobilization as a key to success, pointing out that rehabilitation centers are akin to nursing homes, and reminding patients that their pre-injury functional level will predict their post-injury level.
Most importantly, the tag stresses that patients who go home have better outcomes, underscored by a yellow box emblazoned with the words, “HOME IS BEST.”
A prior study led by Kenneth A. Egol, MD, the Joseph E. Milgram Professor of Orthopedic Surgery, found that patients discharged to home after a hip fracture surgery had fewer complications such as urinary tract infections, acute kidney injuries, and venous thromboembolism. “Dr. Stevens’ successful new educational initiative shows the power of effective messaging in reinforcing that home is the safest recovery space for these patients,” he says.
Consistent Messaging, Encouraging Results
To roll out the initiative, Dr. Stevens met with everyone in contact with the patients, including floor nursing staff, physical and occupational therapists, case managers, social workers, operating room staff, orthopedic residents, orthopedic physician assistants, and hospitalists. She explained the goals of consistent messaging and handed out the badges as a visual reminder.
“Every three months I met with them again to see how it was going and how they felt about it,” she says. Importantly, those in-person meetings allowed her to correct misconceptions, answer questions, and share data on patient outcomes.
“This educational initiative shows the power of effective messaging in reinforcing that home is the safest recovery space for these patients.”
Kenneth A. Egol, MD
Compared to a discharge to home rate of 33.1 percent in a control group of 172 patients, the rate was markedly higher in the badge buddy group of 163 patients, at 47.5 percent. Dr. Stevens says she was heartened to see no accompanying increase in hospital readmissions.
The results, she emphasizes, applied to the relatively stable patients admitted to the orthopedic service at NYU Langone Hospital—Long Island, whereas trauma patients often have more severe conditions and require different considerations.
“This initiative can definitely be expanded to other fracture patients and also to other hospitals within our own system,” she adds; as a follow-up, she’s working to bring the initiative to NYU Langone’s Brooklyn and Suffolk campuses.
One key takeaway, Dr. Stevens says, is engaging with providers who talk to patients the most, including the nursing and physicial therapy staff and patient care technicians. “If you can teach them the messages you want conveyed to patients, I think you’ll have significant improvement in your goals, because they’re the ones who are really interfacing with the patients and their families,” she says.







