Referral Notes:
- As the number of annual TJAs continues to rise, understanding optimal infection prevention techniques is becoming increasingly important.
- In a large prospective randomized controlled trial, researchers showed that there is no significant added benefit from using vancomycin powder, DPI lavage, or both in high-risk patients undergoing TJA, as rates of PJI and wound complications were comparable to a saline control.
- The team is following patients for two years to assess long-term infection rates and clinical implications.
Results of a large prospective randomized trial were recently presented at the 2024 American Association of Hip and Knee Surgeons (AAHKS) Annual Meeting, addressing a longstanding clinical question about use of different infection prevention strategies following high-risk total joint arthroplasty (TJA).
Among patients assigned to one of four infection prevention groups—local vancomycin powder, dilute povidone-iodine (DPI) solution, combination vancomycin-povidone-iodine-protocol (VPIP), or saline control—there were no significant differences in periprosthetic joint infection (PJI) or other surgical outcomes after total hip arthroplasty (THA) or total knee arthroplasty (TKA).
The study was led by Ran Schwarzkopf, MD, professor of orthopedic surgery and director of the Adult Reconstruction Research Center at NYU Langone Health.
“We determined that any of the four infection prevention methods can be safely and effectively utilized by surgeons.”
Ran Schwarzkopf, MD
“Any differences in infection prevention between the groups didn’t bear any clinical significance,” says Dr. Schwarzkopf. “We determined that any of the four infection prevention methods can be safely and effectively utilized by surgeons.”
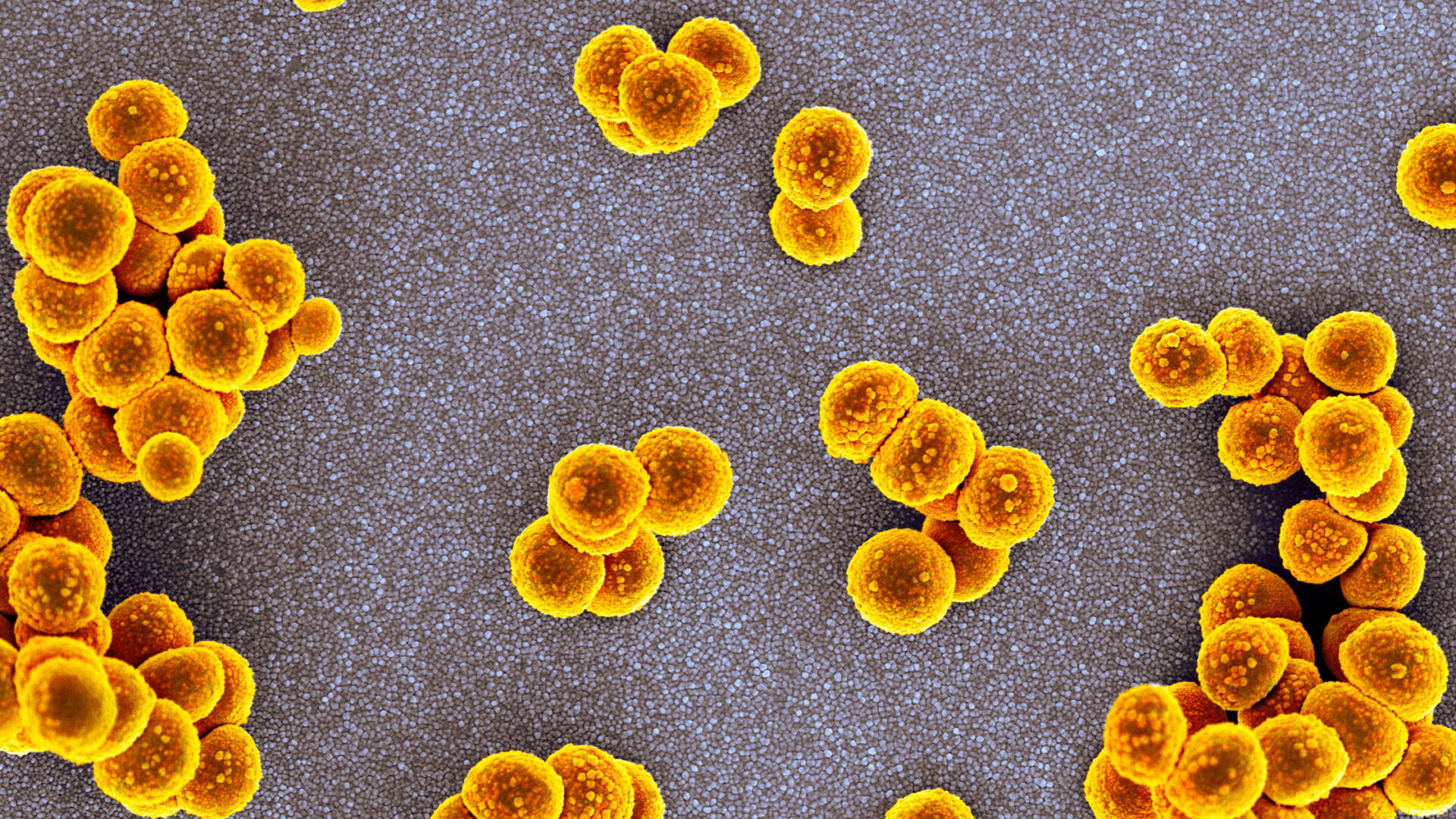
Rare, But Devastating Complication
PJI occurs in approximately 1 to 2.3 percent of primary TJA cases, with some studies reporting rates as high as 5 percent in certain subgroups of higher-risk patients, Dr. Schwarzkopf explains.
Minimizing PJI events is important, he notes, primarily due to significant morbidity and mortality, but also substantial cost burden to healthcare systems. Notably, a diagnosis of PJI confers a higher mortality risk than many common cancers.
“No prospective studies in the orthopedic literature have compared the efficacy of these four perioperative infection prophylaxis strategies on reducing PJI events following TJA,” says Dr. Schwarzkopf. “This is why we undertook the trial.”
Drawing Conclusions from a Large Patient Cohort
The four-arm trial was conducted at 17 high-volume orthopedic surgery centers across the country. A total of 1,901 patients were randomized, 821 and 1,080 in the THA and TKA cohorts, respectively.
After analysis, the researchers found no statistically significant differences in rates of persistent wound drainage or dehiscence, cellulitis or abscess, three-month infection, nor type of septic revisions performed, aseptic revision rates, emergency department (ED) visits, or readmissions between the four groups.
“We thought that we would see at least some degree of added benefit—particularly with the VPIP protocol—compared with saline.”
Given that prior retrospective studies indicated that a combined VPIP protocol could benefit high-risk TKA or THA patients, these findings underscore the importance of conducting large, multicenter prospective studies to validate observational data.
“We thought that we would see at least some degree of added benefit—particularly with the VPIP protocol—compared with saline,” says Dr. Schwarzkopf. The researchers suspect that widespread adoption of modern aseptic practices, including reduced OR traffic and patient preoperative optimization, may help explain the findings.
“Since all of these infection mitigation techniques are inexpensive, we recommend that the choice be left up to surgeon discretion.”
Future Investigations
Dr. Schwarzkopf says that longer follow-up is needed to make any decision on the long-term clinical implications of these results. However, these short-term findings suggest a compelling non-inferiority trend for simplified irrigation protocols, such as saline.
“The study is not finished,” he explains. “Patients are being followed for two years; this analysis focused on infections occurring within the first three months after surgery.”
Future investigations will include comprehensive revision analysis—both aseptic and septic—wound complications, medical complications, ED visits, readmissions, and more. These data will be presented at upcoming meetings.